Chapter: Medical Physiology: Resistance of the Body to Infection: I. Leukocytes, Granulocytes, the Monocyte-Macrophage System, and Inflammation
Inflammation: Role of Neutrophils and Macrophages
Inflammation: Role of Neutrophils and Macrophages
Inflammation
When tissue injury occurs, whether caused by bacteria, trauma, chemicals, heat, or any other phenomenon, multiple substances are released by the injured tissues
This entire complex of tissue changes is called inflammation.
Inflammation is characterized by (1) vasodilation of the local blood vessels, with consequent excess local blood flow; (2) increased permeability of the capillar-ies, allowing leakage of large quantities of fluid into the interstitial spaces; (3) often clotting of the fluid in the interstitial spaces because of excessive amounts of fibrinogen and other proteins leaking from the capil-laries; (4) migration of large numbers of granulocytes and monocytes into the tissue; and (5) swelling of the tissue cells. Some of the many tissue products that cause these reactions are histamine, bradykinin, sero-tonin, prostaglandins, several different reaction prod-ucts of the complement system, reaction products of the blood clotting system, and multiple substances called lymphokines that are released by sensitized T cells Several of these substances strongly activate the macrophage system, and within a few hours, the macrophages begin to devour the destroyed tissues. But at times, the macrophages also further injure the still-living tissue cells.
“Walling-Off” Effect of Inflammation. One of the firstresults of inflammation is to “wall off ” the area of injury from the remaining tissues. The tissue spaces and the lymphatics in the inflamed area are blocked by fibrinogen clots so that after a while, fluid barely flows through the spaces. This walling-off process delays the spread of bacteria or toxic products.
The intensity of the inflammatory process is usually proportional to the degree of tissue injury. For instance, when staphylococciinvade tissues, they release extremely lethal cellular toxins. As a result, inflammation develops rapidly—indeed, much more rapidly than the staphylococci themselves can multi-ply and spread. Therefore, local staphylococcal in-fection is characteristically walled off rapidly and prevented from spreading through the body. Strepto-cocci, in contrast, do not cause such intense local tissue destruction. Therefore, the walling-off process devel-ops slowly over many hours, while many streptococci reproduce and migrate. As a result, streptococci often have a far greater tendency to spread through the body and cause death than do staphylococci, even though staphylococci are far more destructive to the tissues.
Macrophage and Neutrophil Responses During Inflammation
Tissue Macrophage Is a First Line of Defense Against Infection. Within minutes after inflammation begins, the macrophages already present in the tissues, whether histiocytes in the subcutaneous tissues, alveolar macrophages in the lungs, microglia in the brain, or others, immediately begin their phagocytic actions.
When activated by the products of infection and inflammation, the first effect is rapid enlargement of each of these cells. Next, many of the previously sessile macrophages break loose from their attachments and become mobile, forming the first line of defense against infection during the first hour or so. The numbers of these early mobilized macrophages often are not great, but they are lifesaving.
Neutrophil Invasion of the Inflamed Area Is a Second Line of Defense. Within the first hour or so after inflammationbegins, large numbers of neutrophils begin to invade the inflamed area from the blood. This is caused by products from the inflamed tissues that initiate the fol-lowing reactions: (1) They alter the inside surface of the capillary endothelium, causing neutrophils to stick to the capillary walls in the inflamed area. This effect is called margination and is shown in Figure 33–2. (2) They cause the intercellular attachments between the endothelial cells of the capillaries and small venules to loosen, allowing openings large enough for neu-trophils to pass bydiapedesis directly from the blood into the tissue spaces. (3) Other products of inflam-mation then cause chemotaxis of the neutrophils toward the injured tissues, as explained earlier.
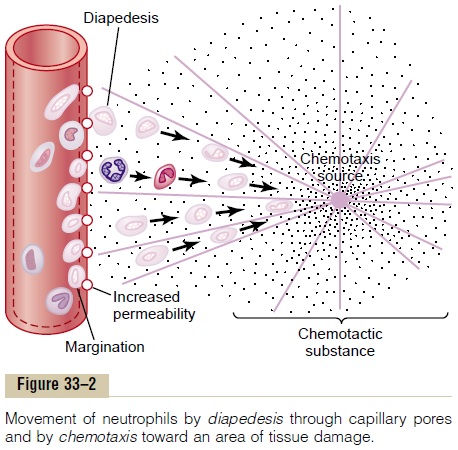
Thus, within several hours after tissue damage begins, the area becomes well supplied with neu-trophils. Because the blood neutrophils are already mature cells, they are ready to immediately begin their scavenger functions for killing bacteria and removing foreign matter.
Acute Increase in Number of Neutrophils in the Blood—“Neu-trophilia.” Also within a few hours after the onset ofacute, severe inflammation, the number of neutrophils in the blood sometimes increases fourfold to five-fold—from a normal of 4000 to 5000 to 15,000 to 25,000 neutrophils per microliter. This is called neu-trophilia, which means an increase in the number ofneutrophils in the blood. Neutrophilia is caused by products of inflammation that enter the blood stream, are transported to the bone marrow, and there act on the stored neutrophils of the marrow to mobilize these into the circulating blood. This makes even more neu-trophils available to the inflamed tissue area.
Second Macrophage Invasion into the Inflamed Tissue Is a Third Line of Defense. Along with the invasion of neutrophils,monocytes from the blood enter the inflamed tissue and enlarge to become macrophages. However, the number of monocytes in the circulating blood is low: also, the storage pool of monocytes in the bone marrow is much less than that of neutrophils. There-fore, the buildup of macrophages in the inflamed tissue area is much slower than that of neutrophils, requiring several days to become effective. Furthermore, even after invading the inflamed tissue, monocytes are still immature cells, requiring 8 hours or more to swell to much larger sizes and develop tremendous quantities of lysosomes; only then do they acquire the full capac-ity of tissue macrophages for phagocytosis. Yet, after several days to several weeks, the macrophages finally come to dominate the phagocytic cells of the inflamed area because of greatly increased bone marrow pro-duction of new monocytes, as explained later.
As already pointed out, macrophages can phagocy-tize far more bacteria (about five times as many) and far larger particles, including even neutrophils them-selves and large quantities of necrotic tissue, than can neutrophils. Also, the macrophages play an important role in initiating the development of antibodies.
Increased Production of Granulocytes and Monocytes by the Bone Marrow Is a Fourth Line of Defense. The fourth line ofdefense is greatly increased production of both gran-ulocytes and monocytes by the bone marrow. This results from stimulation of the granulocytic and mono-cytic progenitor cells of the marrow. However, it takes 3 to 4 days before newly formed granulocytes and monocytes reach the stage of leaving the bone marrow. If the stimulus from the inflamed tissue con-tinues, the bone marrow can continue to produce these cells in tremendous quantities for months and even years, sometimes at a rate 20 to 50 times normal.
Feedback Control of the Macrophage and Neutrophil Responses
Although more than two dozen factors have been implicated in control of the macrophage response to inflammation, five of these are believed to play domi-nant roles. They are shown in Figure 33–6 and consist of (1) tumor necrosis factor (TNF), (2) interleukin-1 (IL-1), (3) granulocyte-monocyte colony-stimulatingfactor (GM-CSF), (4) granulocyte colony-stimulating factor (G-CSF), and (5)monocyte colony-stimulating factor (M-CSF). These factors are formed by activatedmacrophage cells in the inflamed tissues and in smaller quantities by other inflamed tissue cells.
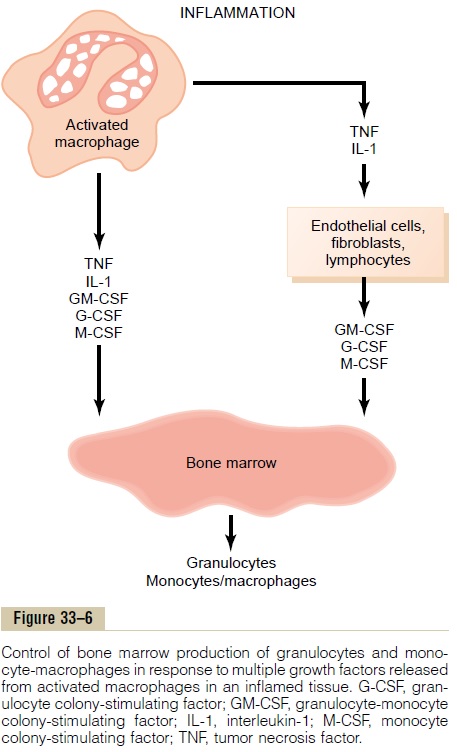
The cause of the increased production of granulo-cytes and monocytes by the bone marrow is mainly the three colony-stimulating factors, one of which, GM-CSF, stimulates both granulocyte and monocyte production; the other two, G-CSF and M-CSF, stimu-late granulocyte and monocyte production, respec-tively. This combination of TNF, IL-1, and colony-stim-ulating factors provides a powerful feedback mecha-nism that begins with tissue inflammation and proceeds to formation of large numbers of defensive white blood cells that help remove the cause of the inflammation.
Formation of Pus
When neutrophils and macrophages engulf large numbers of bacteria and necrotic tissue, essentially all the neutrophils and many, if not most, of the macrophages eventually die. After several days, a cavity is often excavated in the inflamed tissues that contains varying portions of necrotic tissue, dead neu-trophils, dead macrophages, and tissue fluid. This mixture is commonly known as pus.After the infec-tion has been suppressed, the dead cells and necrotic tissue in the pus gradually autolyze over a period of days, and the end products are eventually absorbed
Related Topics