Chapter: Clinical Cases in Anesthesia : The Difficult Airway
Following induction of anesthesia, ventilation by facemask and intubation are impossible. What maneuvers may help?
Following induction of anesthesia, ventilation by facemask and
intubation are impossible. What maneu-vers may help?
Inability to both intubate and ventilate is a
rare occur-rence with a potentially tragic outcome. Several treatment options
exist. A variety of oral and cricoid puncture methods have been described to
assist with such situations.
Of the oral techniques, world-wide experience
is great-est with two: the esophageal-tracheal combitube (ETC) and the
laryngeal mask airway (LMA). The ETC is a device intended for blind insertion
into the airway. It is potentially useful for ventilation and oxygenation
whether located in the esophagus or trachea (Figure 46.4). The ETC is a
dou-ble-lumen tube with an outside diameter of 13 mm. One lumen is open at both
ends, like an endotracheal tube. The other lumen is open at the proximal end
and occluded at the distal end. The ETC contains two inflatable cuffs. The
proximal cuff is large and when situated properly is located in the pharynx,
between the base of the tongue and soft palate. Inflation of this balloon seals
the mouth and nose. A smaller, distal cuff seals the trachea or esopha-gus,
depending upon its location. The lumen with the distal occlusion is perforated
in a segment between the two cuffs.
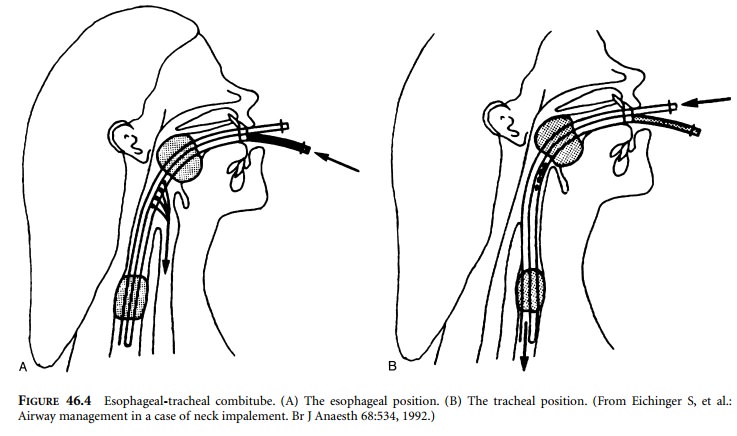
If the ETC is placed in the esophagus, oxygen
is admin-istered through the closed-end lumen, which allows gas to escape from
perforations in the pharyngeal portion (Figure 46.4A). Oxygen then enters the
larynx and is prevented from entering the stomach by the distal balloon. The
proximal balloon prevents gas escaping from the mouth or nose. If the ETC is
placed into the trachea, oxygen is administered into the lumen open at both
ends, which functions like a standard endotracheal tube (Figure 46.4B). The
ETC, when placed in the esophagus, allows suctioning of gastric contents
through the open-ended side, thereby helping to reduce the risk of aspiration
pneumonitis. In the esophageal position, pulmonary toilet is impossible through
the ETC.
Ventilation through the ETC has been adequate
during anesthesia, intensive care, cardiopulmonary resuscitation, and
mechanical ventilation. It has been used successfully to oxygenate and
ventilate patients whose trachea could not be intubated and whose lungs could
not be ventilated by facemask. At the time of this writing, it is available in
two adult sizes.
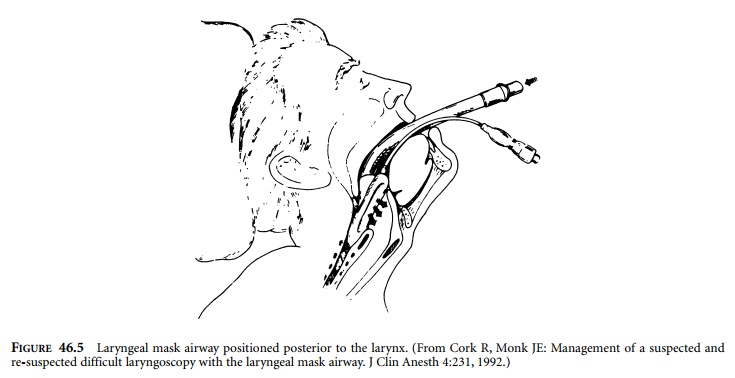
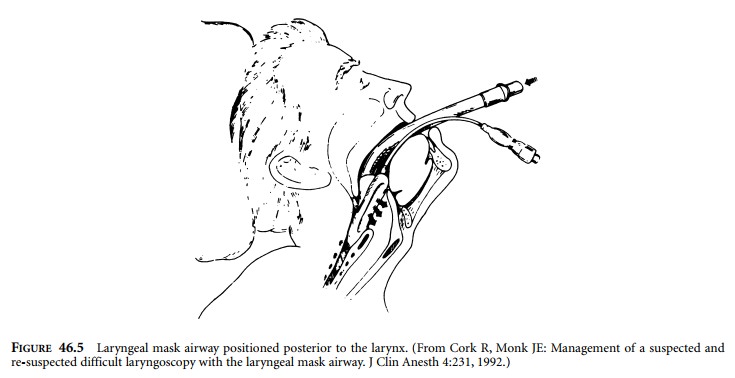
Another device that is inserted blindly through
the mouth is the LMA (Figure 46.5). The LMA is a 12-mm inner diameter tube
attached to a mask. The mask has an inflatable balloon around its periphery.
With the balloon deflated, the mask is advanced into the mouth and through the
airway until obstruction to passage is encountered. At this point, the mask
should be positioned cephalad to the esophagus and surrounding the larynx. The
balloon is inflated in an attempt to create an airtight chamber around the
larynx. The 12-mm tube now exits from the mouth and is connected to an anesthesia
breathing circuit.
The LMA is available in adult and pediatric
sizes. It works well in 90–98% of cases. This 2–10% failure rate is far greater
than the incidence of inability to ventilate and intubate. Nevertheless, it has
been successfully used for air-way management in elective surgery, as well as
in cases of predicted and unanticipated difficult intubation. The LMA has been
used to assist blind intubation and FFL-guided intubation in patients whose
larynxes could not be visual-ized by traditional rigid laryngoscopy.
If the LMA’s inflatable balloon is not
positioned prop-erly, a large gas leak occurs around the mask, impairing
ventilation. This leak is exacerbated by high inflation pres-sures. Malposition
of the balloon increases the risk of gastric content aspiration into the lungs.
Obstruction to gas flow may occur if the tongue or epiglottis is pushed back
over the larynx as the mask is inserted. Difficulty in positioning the LMA
occurred 18% of the time, and failure to properly position occurred 3% of the
time. It will pre-dictably offer little in cases of airway stenosis and gross
anatomic distortion. LMAs are available in several vari-eties. The classic LMA
is shown in Figure 46.5. A disposable model also exists. Advantages of
disposable models include reduced cost for each one, as well as elimination of
cross-contamination from inadequately cleaned and sterilized, reusable types.
An intubating LMA was designed to facili-tate tracheal tube passage through the
glottis. Although it works well to maintain upper airway patency, ideal
align-ment with the trachea can be problematic. Deviations from ideal
positioning hamper tracheal tube passage. The ProSeal LMA comes equipped with a
distal port. The port is positioned just cephalad to the esophagus and allows
egress of gastric contents that might collect in the pharynx.
A tube connected to the port provides access to
the open-ing. With proper alignment, a gastric tube can be inserted through the
ProSeal LMA and into the stomach for elimi-nation of gastric contents.
Alternative supraglottic devices include
COBRAs, pha-ryngeal airways, E-Z Tubes, Chou Airways, and others.
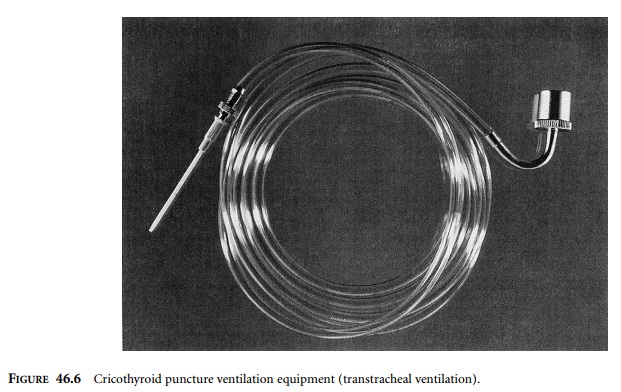
Of the more invasive techniques, cricothyroid
puncture and transtracheal ventilation are well described. Successful use of
transtracheal ventilation relies on preparation before the critical incident
occurs. Equipment must be assembled and readily available to patients requiring
its use. Devices are best stored in all anesthetizing locations and anywhere
intubation might reasonably be anticipated.
Basic equipment consists of a 14-gauge
over-the-needle catheter with luer lock adapter, non-compressible oxygen
tubing, standard 15-mm connector, and a source of pres-surized oxygen (Figure
46.6). Such systems deliver gas at very high pressures and tend to disconnect
at portions that are not securely fastened.
With the patient in the supine position, the
head is extended to expose the anterior neck. The thyroid cartilage is palpated
and the finger run inferiorly until a depression (the cricothyroid membrane) is
felt. Another dense substance (cricoid cartilage) is appreciated just caudad to
the depres-sion. A 14-gauge needle is placed through the skin perpen-dicular to
all planes, and advanced until the cricothyroid membrane is punctured. Proper
positioning within the trachea is confirmed by freely aspirating air through
the needle. The needle is then removed, leaving the catheter positioned in the
lumen of the trachea. The device is attached to the intravenous catheter and
100% oxygen administered under positive pressure. This is most con-veniently
accomplished by attaching the 15-mm connector to the anesthesia machine’s
common gas outlet and con-trolling the flow of oxygen with the oxygen flush
valve. Not all anesthesia machines function well in this circumstance.
Ventilation systems utilizing pressure
step-down valves interposed between high-pressure oxygen sources, such as wall
oxygen or oxygen tanks, can be attached to the same cricothyroid puncture
catheter. The higher the pressure generated, the more likely the catheter will
become dislodged, so a designated holder must be assigned to keep it in place.
If intubation and ventilation are impaired by
tissues encroaching on the airway, then rigid bronchoscopy may pro-vide for
immediate life-saving ventilation and oxygenation.
Related Topics