Chapter: Medical Physiology: Cardiac Failure
Dynamics of Severe Cardiac Failure- Decompensated Heart Failure
Dynamics of Severe Cardiac Failure- Decompensated Heart Failure
If the heart becomes severely damaged, no amount of compensation, either by sympathetic nervous reflexes or by fluid retention, can make the excessively weak-ened heart pump a normal cardiac output. As a con-sequence, the cardiac output cannot rise high enough to make the kidneys excrete normal quantities of fluid. Therefore, fluid continues to be retained, the person develops more and more edema, and this state of events eventually leads to death. This is called decom-pensated heart failure. Thus, the main cause of decom-pensated heart failure is failure of the heart to pump sufficient blood to make the kidneys excrete daily the necessary amounts of fluid.
Graphical Analysis of Decompensated Heart Failure. Figure22–2 shows greatly depressed cardiac output at differ-ent times (points A to F) after the heart has become severely weakened. Point A on this curve represents the approximate state of the circulation before any compensation has occurred, and point B, the state a few minutes later after sympathetic stimulation has compensated as much as it can but before fluid reten-tion has begun. At this time, the cardiac output has risen to 4 L/min and the right atrial pressure has risen to 5 mm Hg. The person appears to be in reasonably good condition, but this state will not remain stable because the cardiac output has not risen high enough to cause adequate kidney excretion of fluid; therefore, fluid retention continues and can eventually be the cause of death. These events can be explained quanti-tatively in the following way.
Note the straight line in Figure 22–2, at a cardiac output level of 5 L/min. This is approximately the crit-ical cardiac output level that is required in the normal adult person to make the kidneys re-establish normal fluid balance—that is, for the output of salt and water to be as great as the intake of these. At any cardiac output below this level, all the fluid-retaining mecha-nisms discussed in the earlier section remain in play and the body fluid volume increases progressively. And because of this progressive increase in fluid volume, the mean systemic filling pressure of the
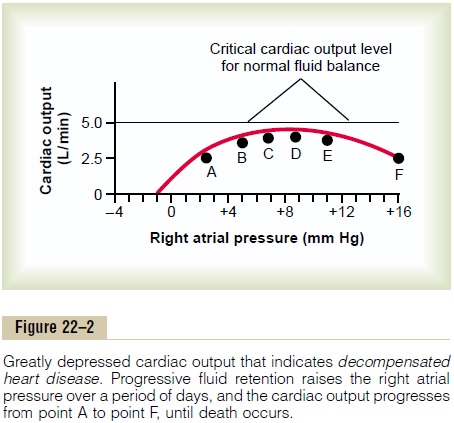
circulation continues to rise; this forces progressively increasing quantities of blood from the person’s peripheral veins into the right atrium, thus increasing the right atrial pressure. After 1 day or so, the state of the circulation changes in Figure 22–2 from point B to point C—the right atrial pressure rising to 7 mm Hg and the cardiac output to 4.2 L/min. Note again that the cardiac output is still not high enough to cause normal renal output of fluid; therefore, fluid continues to be retained. After another day or so, the right atrial pressure rises to 9 mm Hg, and the circulatory state becomes that depicted by point D. Still, the cardiac output is not enough to establish normal fluid balance.
After another few days of fluid retention, the right atrial pressure has risen still further, but by now, cardiac function is beginning to decline toward a lower level.This decline is caused by overstretch of the heart, edema of the heart muscle, and other factors that diminish the heart’s pumping performance. It is now clear that further retention of fluid will be more detrimental than beneficial to the circulation. Yet the cardiac output still is not high enough to bring about normal renal function, so that fluid retention not only continues but accelerates because of the falling cardiac output (and falling arterial pressure that also occurs). Consequently, within a few days, the state of the circulation has reached point F on the curve, with the cardiac output now less than 2.5 L/min and the right atrial pressure 16 mm Hg. This state has approached or reached incompatibility with life, and the patient dies. This state of heart failure in which the failure continues to worsen is called decompensatedheart failure.
Thus, one can see from this analysis that failure of the cardiac output (and arterial pressure) to rise to the critical level required for normal renal function results in (1) progressive retention of more and more fluid, which causes (2) progressive elevation of the mean systemic filling pressure, and (3) progressive elevation of the right atrial pressure until finally the heart is so overstretched or so edematous that it cannot pump even moderate quantities of blood and, therefore, fails completely. Clinically, one detects this serious condi-tion of decompensation principally by the progressing edema, especially edema of the lungs, which leads to bubbling rales in the lungs and to dyspnea (air hunger). All clinicians know that lack of appropriate therapy when this state of events occurs leads to rapid death.
Treatment of Decompensation. The decompensationprocess can often be stopped by (1) strengthening theheart in any one of several ways, especially by admin-istration of a cardiotonic drug, such as digitalis, so that the heart becomes strong enough to pump adequate quantities of blood required to make the kidneys func-tion normally again, or (2) administering diuretic drugsto increase kidney excretion while at the same timereducing water and salt intake, which brings about a balance between fluid intake and output despite low cardiac output.
Both methods stop the decompensation process by re-establishing normal fluid balance, so that at least as much fluid leaves the body as enters it.
Mechanism of Action of the Cardiotonic Drugs Such as Digitalis. Cardiotonic drugs, such as digitalis, whenadministered to a person with a healthy heart, have little effect on increasing the contractile strength of the cardiac muscle. However, when administered to a person with a chronically failing heart, the same drugs can sometimes increase the strength of the failing myocardium as much as 50 to 100 per cent. Therefore, they are one of the mainstays of therapy in chronic heart failure.
Digitalis and other cardiotonic glycosides are believed to strengthen heart contraction by increasing the quantity of calcium ions in muscle fibers. In the failing heart muscle, the sarcoplasmic reticulum fails to accumulate normal quantities of calcium and, therefore, cannot release enough calcium ions into the free-fluid compartment of the muscle fibers to cause full contraction of the muscle. One effect of dig-italis is to depress the calcium pump of the cell mem-brane of the cardiac muscle fibers. This pump normally pumps calcium ions out of the muscle. However, in the case of a failing heart, extra calcium is needed to increase the muscle contractile force. Therefore, it is usually beneficial to depress the calcium pumping mechanism a moderate amount using digitalis, allow-ing the muscle fiber intracellular calcium level to rise slightly.
Related Topics