Chapter: Essentials of Psychiatry: Childhood Disorders: Communication Disorders
Diagnosis - Childhood Disorders: Communication Disorders
Diagnosis
Phenomenology
Expressive Language Disorder
This condition varies with age and severity.
Vocabulary, word-finding, sentence length, variety of expression and
grammatical complexity may all be reduced. Most children with the
develop-mental subtype of this disorder demonstrate delayed language
development. Often auxiliary words or prepositions are omitted, resulting in
telegraphic speech: “he was going to school” becomes “he going school”. Word
order may be garbled: “Him like too me” for “I like him, too”. Words or phrases
may be repeated to the degree that speech may be echolalic, perseverative, or
both. Con-versation may be tangential, with sudden inappropriate changes of
topic, or conversely, perseveration. Pragmatic difficulties, such as in
initiating or terminating conversations, are seen, as is avoidance of
conversation. These children frequently are regarded as socially inappropriate
or inept, and at times may be suspected of having a formal thought disorder or
a Pervasive Developmental Disorder. They frequently have academic problems
because of their diffi-culty in responding verbally to exercises. They may have
motor coordination problems and various other neurodevelopmental
ab-normalities, documented upon neurological examination, EEG, or neuroimaging,
although no consistent patterns are seen.
Mixed Receptive-expressive Language Disorder
Children with this disorder may have all the
problems of Expres-sive Language Disorder. In addition, they do not understand
all that they hear. The deficits may be mild or severe, and at times
deceptively subtle, since patients may conceal them or avoid in-teraction. All
areas and levels of language comprehension may be disturbed. Thus the child may
not understand speech that is rapid, certain words or categories of words, such
as abstract quan-tities, or types of statements, such as conditional clauses.
These children may seem not to hear or attend, or to misbehave by not following
commands correctly. At times, when conversation is redirected to them in a
slower or more concise fashion, they may understand and respond belatedly, and
thereby be accused of willful avoidance. More severely impaired children may
not fol-low the rules of syntax or word order, and thus confuse subjects and
objects or questions and declarations. Often in more severe cases, disabilities
may be multiple and pervasive, affecting pro-cessing, recall and association.
Such deficits have immense social consequences.
Phonologic Disorders
This category is characterized by persistent errors
in the pro-duction of speech. These include omission, substitution or
dis-tortion of sounds. Omissions include single or multiple sounds: “I go o coo
o the but” (I go to school on the bus); or “I re a boo” (I read a book).
Substitutions include w/l, t/s, w/r, and d/g
“I taw a wittle wed wadio. It pwayed dood music”. Lisping, the frontal
or lateral misarticulation of sibilants, is a common distortion. Defects in the
order of sounds or insertions of extra-neous sounds may also be heard: “catht”
for “cats”. The occur-rence of these errors is persistent but not constant.
Usually only some sounds are affected. Some articulation errors are expected in
early childhood, especially involving sounds that are usually mastered at a
later age (in English, /l/, /r/, /s/, /z/, /th/, /ch/); these errors are not
regarded as pathological unless they persist and result in adverse consequences
to the individual. Ninety percent or more of children have mastered the more
difficult sounds by age 6 to 8.
Stuttering
Stuttering is the most easily recognized
communication disorder. It varies in severity among individuals. It may vary
over time and circumstance. It is typically more severe when the affected child
is stressed or anxious, and especially when communication is ex-pected. Because
of its often gradual onset, children are at first frequently not aware of its
presence. Over time they may become more anxious and withdraw from
conversation, as the degree of social discrimination they experience increases.
Stuttering may be accompanied by various movements which may seem either to
express or discharge anxiety, such as blinking, grimacing, or hyperventilation.
Children who stutter may sing or talk to them-selves without difficulty.
Sometimes children may attempt to stop stuttering by slowing down or pausing in
their speech; but this is frequently unsuccessful and leads to an exacerbation.
Thus a pat-tern of habitual fear and avoidance emerges.
Communication Disorder Not Otherwise Specifi ed
This category, used to include disorders that do
not fit the criteria for any of the other Communication Disorders, is generally
used only to describe disorders of voice, including pitch, intonation, volume,
or resonance. Hyponasality is characterized by the “ad-enoidal” speech
simulated by speaking with the nose pinched. Hypernasality, secondary to
velopharyngeal insufficiency, may be associated with serious voice problems.
Air escapes into the nasal cavity, resulting in nasal air emission, snorting or
a nasal grimace during speech.
Assessment
Interview and Observation
The psychiatrist seeing children must be familiar
with normal milestones of speech and language development and ask the parents
or guardians about the child’s speech and language, both past and current. Much
can be learned from even a few questions: Does the child seem to hear and
understand what is being said? Does the child require visual prompts? Does the
child in fact use spoken language to communicate? How long and complicated are
his sentences? Does the child “make sense” to outsiders? Can she be clearly
understood, even by strangers? Which sounds does the child find difficult? Does
the child use unusual volume, pitch, or nasality? Does he observe the rules of
conversation? Parent–child communication should also be observed.
For younger children, assessment may best be
carried out in a play situation. Rutter (1987) recommends that the clinician
assess inner language, comprehension, production, phonation and pragmatics.
Inner language means symbolization, which may be observed in the child’s
representational use of play ma-terials. Comprehension is assessed through
conversation and the use of developmentally appropriate questions and commands,
especially with nonverbal augments or prompts. The clinician should note how
well a child can follow and draw inferences from a conversation. Production
refers to speech, its fluency and intel-ligibility. Pragmatics are those
aspects of language that render it useful for social communication beyond the
most concrete level. Does the child appreciate the nuances of her partner’s
conver-sation, as, for example, when they signal beginnings and end-ings of
conversations, topic changes, or the patient’s turn to talk? Pragmatic language
involves nonverbal elements. Deficiencies in this area impair abstraction and
may render the individual almost “robot-like”.
In all cases, observations should be made in as
relaxed a fashion as possible, avoiding interrogation or rote exercises. If a
child fails to communicate a given item, necessary help, in-cluding nonverbal
prompts, should be offered, so that the child has the experience of success. A
sense of failure will stifle communication.
All of the phenomena seen in a clinical interview
may also be pursued in school settings, and teacher input is essential in the
evaluation of these children.
Developmental and Cultural Influences
The need for a clinician to be aware of normal
developmental expectations has been cited. Special sensitivity must be
exer-cised for the range of accents, dialects and conversational styles encountered.
English is spoken in an extraordinary range of patterns even within each
dialect group. It is essential that one does not pathologize differences in
intonation or dialect. Many American children grow up in multilingual
environments, and speak with a synthesis of languages, especially during their
pre-school years. Finally, children of minority groups who have suf-fered
social discrimination and children who live in physically dangerous
environments may necessarily be cautious and less forthcoming with language;
this may be adaptive in some cases and not a disorder at all.
Differential Diagnosis
Expressive Language Disorders and Mixed Receptive-expressive Disorders
These disorders are distinguished from each other by the pres-ence or absence of receptive problems. Children with autism may have any or all of the characteristics of the language disorders. However, they have many additional problems including the use of language in a restricted and often ste-reotypic fashion, rather than for communicative purposes. They also have difficulties with a wider range of interactions with persons and objects in their environment, and exhibit a restricted range of behaviors. The language impairments of mental retardation, oral-motor deficits, or environmenta deprivation are not diagnosed in this category unless they are well in excess of what is expected. Language impairment due to environmental deprivation tends to improve dramatically with environmental improvement. Sensory deficits, especially hearing impairment, may restrict language development. Any indication of potential hearing impairment, no matter how tenuous, should prompt a referral for an audiologic evalua-tion. Obviously, hearing and language disorders can and do coexist. Some children develop an acquired aphasia as a com-plication of general medical illness. This condition is usually temporary; only if it persists beyond the acute course of the medical illness is a language disorder diagnosed. A very se-vere acquired language disorder is seen in Landau-Kleffner Syndrome (acquired epileptic aphasia), accompanied by sei-zures and other CNS dysfunctions, and usually occurring between the ages of three and nine.
Phonological Disorder and Stuttering
The conditions should be distinguished from normal
dysfluen-cies in young children. For example, misarticulation of some sounds,
such as /l/, /r/, /s/, /z/, /th/, and /ch/, is common among pre-schoolers and
resolves with age. As with the language disorders, these diagnoses are given in
the case of motor of sensory deficit, mental retardation, or environmental
deprivation only if the dis-order is much more severe than expected in these
conditions. Problems limited to voice alone are included under Communica-tion
Disorder NOS.
Formal Speech and Language Assessment
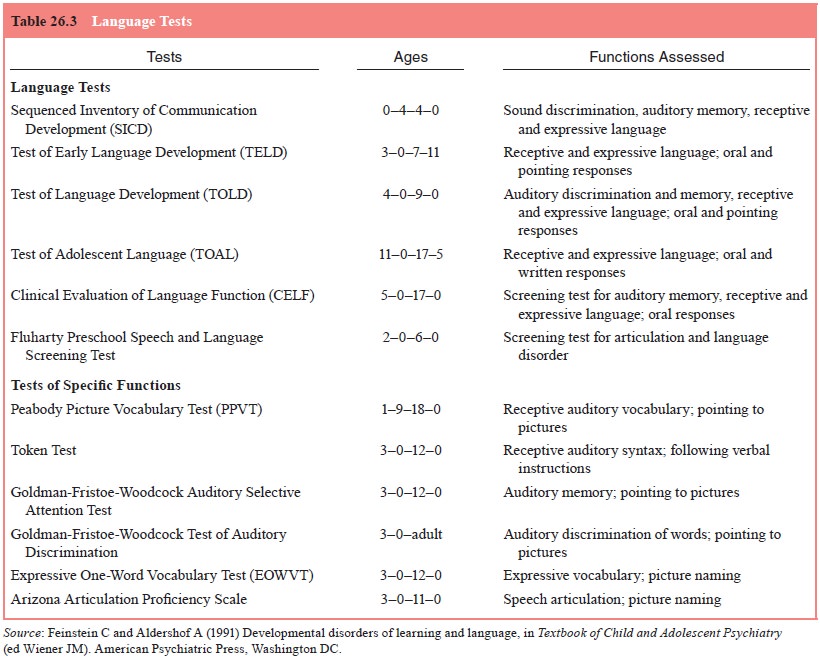
A number of instruments are available for the
assessment of communication. Some of these are listed in Table 26.3. Most are
beyond the training of physicians, whose most important con-tributions are
interview skills and medical assessment; but a fa-miliarity with them can help
the physician develop a repertoire and knowledge of screening measures. Because
of the complex comorbidity of these disorders, they are often best assessed by
an interdisciplinary team (McKirdy, 1985; Klykylo, 2005). The team’s activities
are usually coordinated by a case manager, of-ten a pediatrician or a child and
adolescent psychiatrist. Often the team includes an audiologist, a
psychologist, medical special-ists including pediatric neurologists and
otorhinolaryngolists, an educational specialist or liaison special educator,
and a speech and language pathologist.
The speech and language pathologist (SLP) has a
gradu-ate professional degree and should be certified by The American
Speech, Language and Hearing Association (ASHA).
The SLP uses a combination of interview techniques, behavioral observations and
standardized instruments to identify Communication Disor-ders, as well as
patterns of communication that are not pathologic. The assessment of an SLP is
usually the definitive measure of the presence or absence of a Communication
Disorder. Families may consult an SLP directly or be referred by other
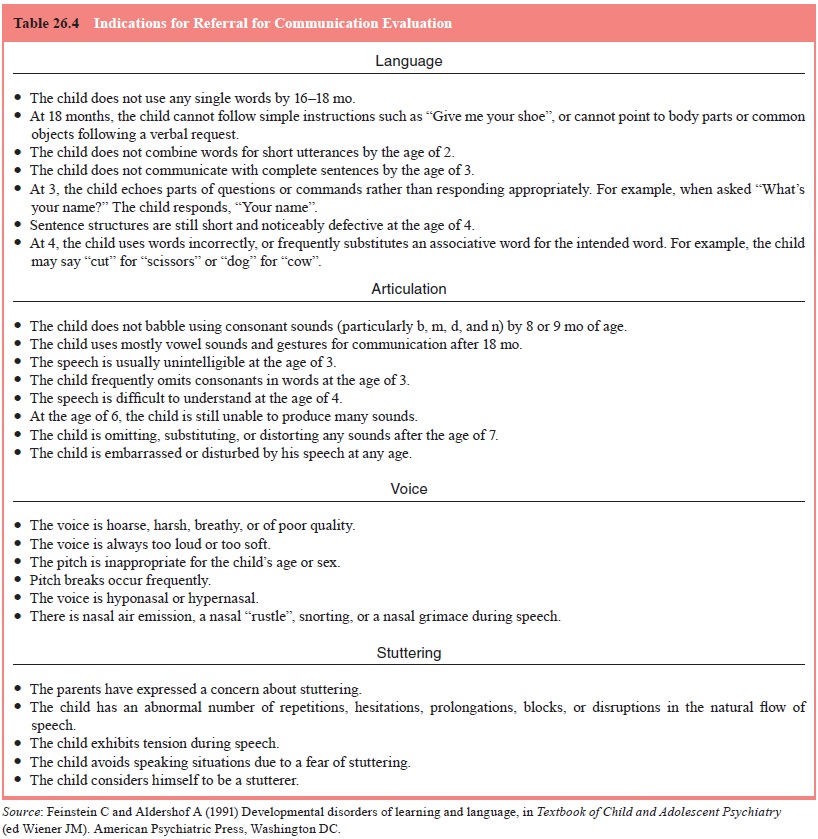
clinicians. The responsibility of psychiatrists and other professionals in this
process is simple and straightforward: any suspicion of any com-munication
problem in any patient should prompt referral to a qualified SLP. Even when a
disorder appears to be limited and benign, communication evaluation by an SLP
can disclose subtle impairments that could have profound consequences. Table
26.4 lists indication for referral.
Related Topics