Chapter: Clinical Cases in Anesthesia : Anesthesia For Nonobstetric Surgery During Pregnancy
What is a teratogen and which anesthetic agents are known teratogens?
What is
a teratogen and which anesthetic agents are known teratogens?
A teratogen is a substance that produces an
increase in the incidence of a particular defect that cannot be attributed to
chance. In order to produce a defect, the teratogen must be administered in a
sufficient dose at a critical point in development. In humans, this critical
point is during organogenesis, which extends from 15 days to approximately 60
days gestational age. However, the central nervous system does not fully
develop until after birth; therefore the critical time for this system may
extend beyond gestation.
Three approaches have been utilized to study
the effects of anesthetic agents or anesthesia in the pregnant patient:
animal
studies, (2) studies of operating room personnel chronically exposed to trace
concentrations of inhaled anes-thetics, and (3) studies of women who underwent
surgery while pregnant.
The results of animal studies are of limited
value because of (1) species variation, (2) the fact that the doses of
anesthetic agents used in animal studies were usually far greater than those
used clinically, and (3) other factors such as hypercarbia, hypothermia, and
hypoxemia (known teratogens) were either not measured or not controlled.
Species variation is particularly important. Thalidomide has no known
teratogenic effects on rats and was approved by the United States Food and Drug
Administration (FDA) for use in humans. It is now known that thalidomide is
teratogenic in humans.
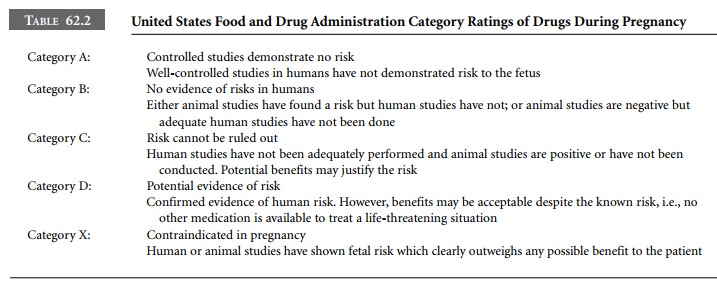
The FDA has established a risk classification
system to assist physicians in weighing the risks and benefits when choosing
therapeutic agents for the pregnant woman (Table 62.2). Most anesthetic agents,
including the intra-venous induction agents, local anesthetics, opioids, and
neuromuscular blocking drugs have been assigned a Category B or C
classification (Table 62.3).
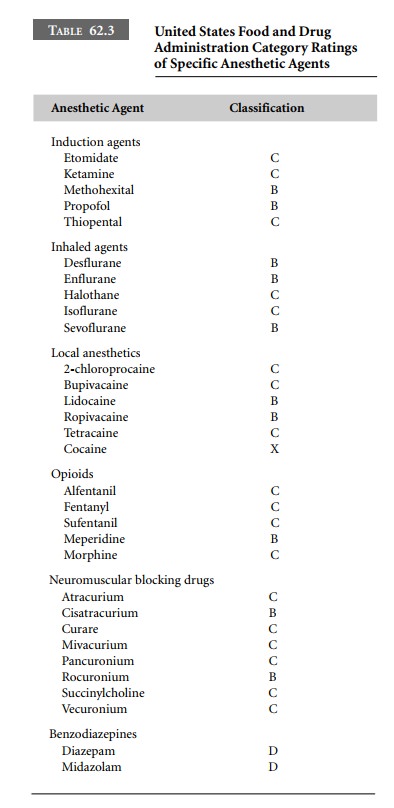
The use of two commonly used agents,
benzodiazepines and nitrous oxide, are controversial. Some investigators, in
retrospective studies, noted an association between diazepam taken in the first
6 weeks of pregnancy and cleft palate. Although this finding has been
questioned by the results of a prospective study, diazepam and other
benzodi-azepines are classified by the FDA as Category D drugs (i.e., positive
evidence of risk) and, therefore, should be avoided.
Nitrous oxide is a known teratogen in mammals.
The presumption was that the teratogenicity of nitrous oxide in animals is
related to its oxidation of vitamin B12, which then cannot function
as a cofactor for the enzyme methionine synthetase. Methionine synthetase is
needed for the forma-tion of thymidine, a subunit of DNA. However, pretreat-ment
of rats exposed to nitrous oxide with folinic acid, which bypasses the
methionine synthetase step in DNA synthesis, does not prevent congenital
abnormalities. In addition, suppression of methionine synthetase occurs at low
concentrations of nitrous oxide – concentrations found safe in animal studies.
Despite these theoretical concerns, nitrous oxide has not been found to be
associated with congenital abnormalities in humans. Interestingly, the FDA has
not given nitrous oxide a category classification because it is a medical gas
and not directly regulated by the FDA.
A number of epidemiologic studies have been
performed to determine the health hazards, including birth defects and
spontaneous abortions, of chronic exposure to anes-thetic gases. All the
studies found similar results. The authors of the largest study, sponsored by
the American Society of Anesthesiologists (1974), sent questionnaires to 73,496
individuals who may have been exposed to anesthetic gases. The study population
included the entire membership of the American Society of Anesthesiologists,
the American Association of Nurse Anesthetists, the Association of Operating
Room Nurses, and the Association of Operating Room Technicians. These personnel
(anesthesiologists, nurses, etc.) received questionnaires in the mail designed
to gather information about the extent of their exposure and reproductive
outcome. They found that operating room personnel had an increased risk of
spontaneous abortions and congenital abnormalities. They recommended that a
means to scavenge trace anesthetic gases should be manda-tory in all operating
rooms, which is the current standard. However, all these studies were later
criticized for their lack of a control group, low response rate to
questionnaires, recall bias, and statistical inaccuracies.
There have also been several retrospective
studies of pregnant patients who had undergone surgery to deter-mine whether
there is an association between anesthesia and surgery and congenital defects,
spontaneous abor-tions, or fetal demise. All studies have found similar
results. In the largest study, Mazze and Kallen (1989) linked the data from
three Swedish health registries: the Medical Birth Registry, the Registry of
Congenital Malformations, and the Hospital Discharge registry for the 9-year
period 1973–1981. They examined the data for four adverse out-comes including
congenital defects, stillborn infants, infants born alive but who died within 7
days, and infants with a birth weight < 1,500 grams and < 2,500 grams. They found 5,405 of 720,000 women
had undergone surgery during their pregnancy. In their data set, most
procedures were per-formed during the first trimester (41.6%), and the
incidence decreased during the second (34.8%) and third (23.5%) trimesters.
There was no increase in babies with congenital abnormalities or stillborn
births among those who underwent surgery while pregnant during any trimester.
However, the number of babies born with a birth weight < 1,500 grams and < 2,500 grams, and the number
of babies who died within 7 days of birth, was greater in those who underwent
surgery while pregnant. This was true during all three trimesters. These risks
could not be linked to either the specific anesthetic agents or the anesthetic
technique. Most operations (54%) were performed under general anesthe-sia and
nitrous oxide was used in 98% of the general anes-thetics. The increased risk
to the fetus may be due to the condition that necessitated surgery in the first
place, with the highest rate occurring with gynecologic procedures. These data
are very important because they clearly demon-strate that anesthetic agents are
not teratogenic and that the greatest risk is premature labor with the delivery
of a low birth weight baby. Furthermore, the data strongly sug-gest that the
anesthetic agents are not responsible for the major complication of surgery:
premature labor and early delivery of the fetus.
Related Topics