Chapter: Psychiatric Mental Health Nursing : Therapeutic Communication
Verbal Communication Skills
VERBAL COMMUNICATION SKILLS
Using Concrete Messages
When speaking to the client the nurse should use words that are as
clear as possible so that the client can understand the message. Anxious people
lose cognitive processing skills—the higher the anxiety, the less the ability
to process concepts—so concrete messages
are important for accurate information exchange. In a concrete message, the
words are explicit and need no interpretation; the speaker uses nouns instead
of pronouns—for example, “What health symptoms caused you to come to the
hospital today?” or “When was the last time you took your antidepressant
medications?” Concrete questions are clear, direct, and easy to understand.
They elicit more accurate responses and avoid the need to go back and rephrase
unclear questions, which interrupts the flow of a therapeutic interaction.
Abstract messages, in contrast, are unclear
patterns of words that often contain
figures of speech that are difficult to interpret. They require the listener to
interpret what the speaker is asking. For example, a nurse who wants to know
why a client was admitted to the unit asks, “How did you get here?” This is an
abstract message: the terms how and here are vague. An anxious client might
not be aware of where he or she is and might reply, “Where am I?” or might
interpret this as a question about how he or she was conveyed to the hospital
and respond, “The ambulance brought me.” Clients who are anxious, from
different cul-tures, cognitively impaired, or suffering from some mental
disorders often function at a concrete level of comprehen-sion and have
difficulty answering abstract questions. The nurse must be sure that statements
and questions are clear and concrete.
The following are examples of abstract and concrete messages:
Abstract (unclear): “Get the stuff from him.”
Concrete (clear): “John will be home today at 5 pm, and you can pick up your clothes at that
time.”
Abstract (unclear): “Your clinical perfor-mance has to improve.”
Concrete (clear): “To administer medications tomorrow, you’ll have to be able to calculate dosages correctly
by the end of today’s class.”
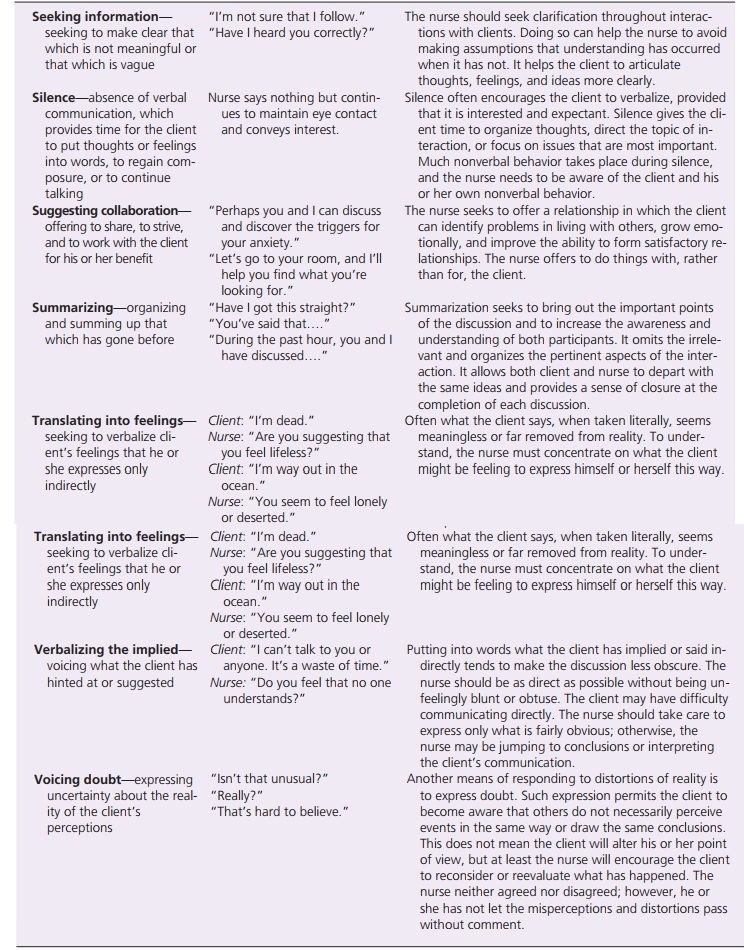
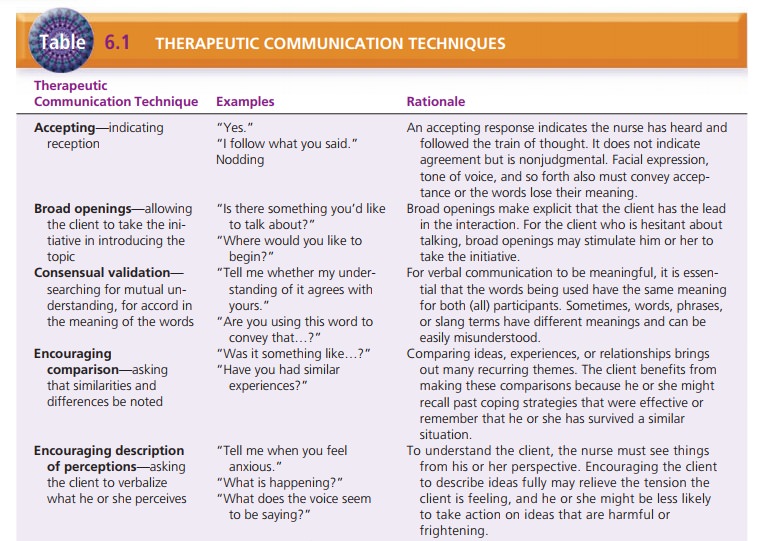
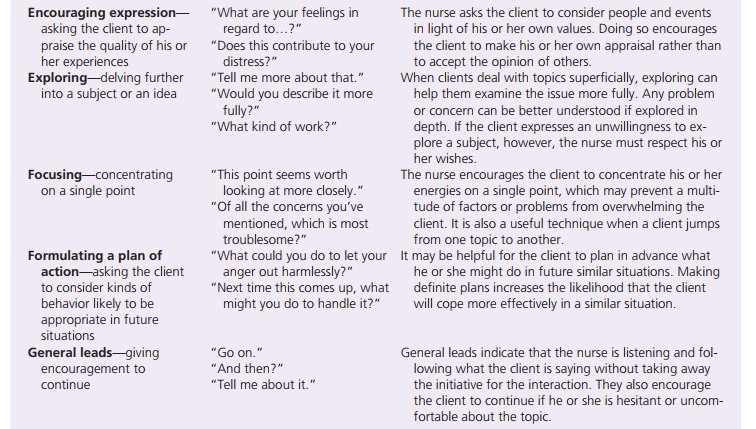
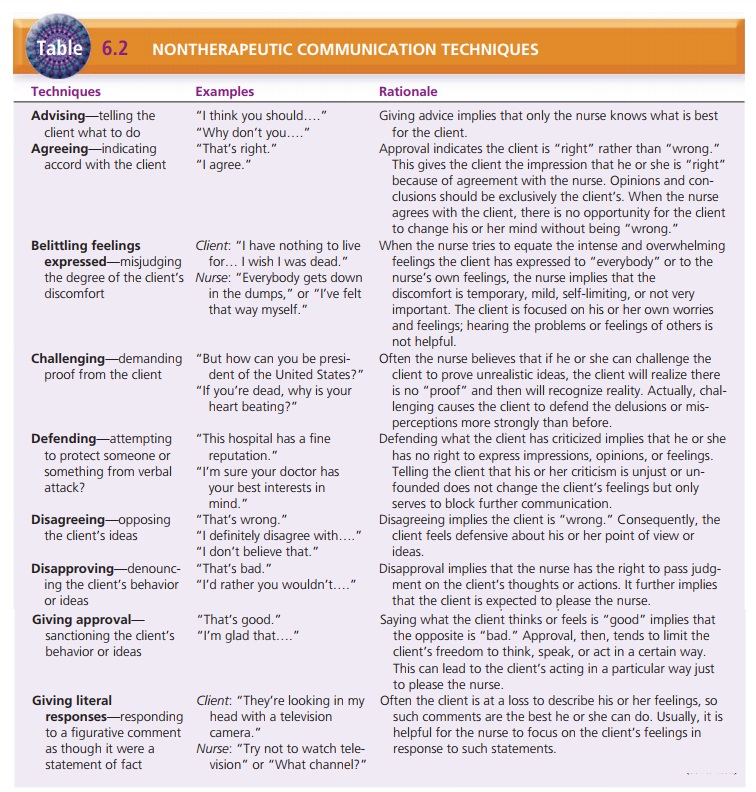
Using Therapeutic Communication Techniques
The nurse can use many therapeutic communication tech-niques to
interact with clients. The choice of technique depends on the intent of the
interaction and the client’s ability to communicate verbally. Overall, the
nurse selects techniques that facilitate the interaction and enhance
com-munication between client and nurse. Table 6.1 lists these techniques and
gives examples. Techniques such as![]()
![]() exploring, focusing, restating, and reflecting
encourage the client to discuss his or her feelings or concerns in more depth.
Other techniques help focus or clarify what is being said. The nurse may give
the client feedback using tech-niques such as making an observation or
presenting reality.
exploring, focusing, restating, and reflecting
encourage the client to discuss his or her feelings or concerns in more depth.
Other techniques help focus or clarify what is being said. The nurse may give
the client feedback using tech-niques such as making an observation or
presenting reality.
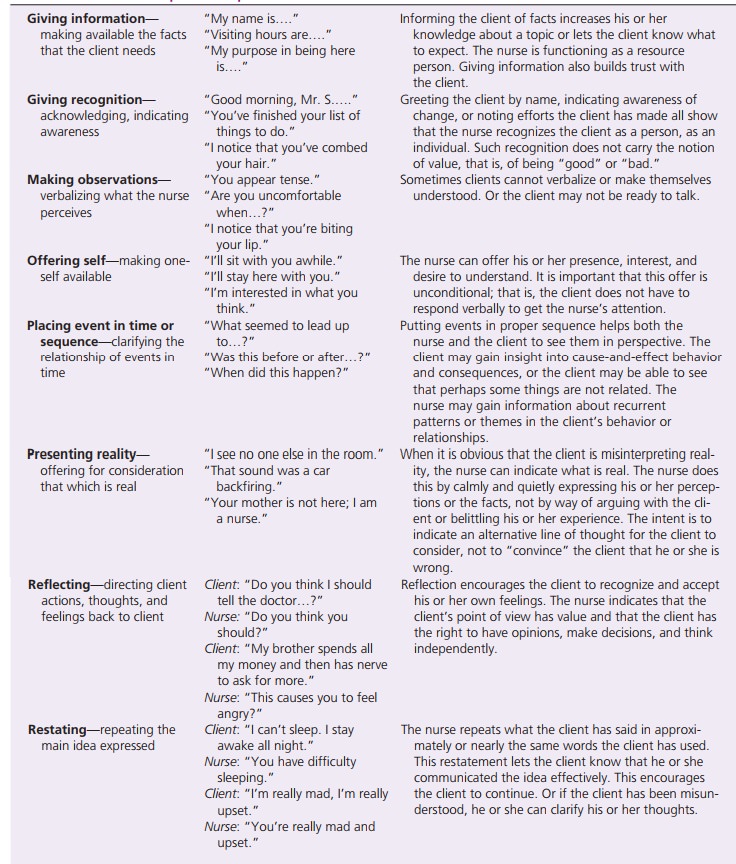
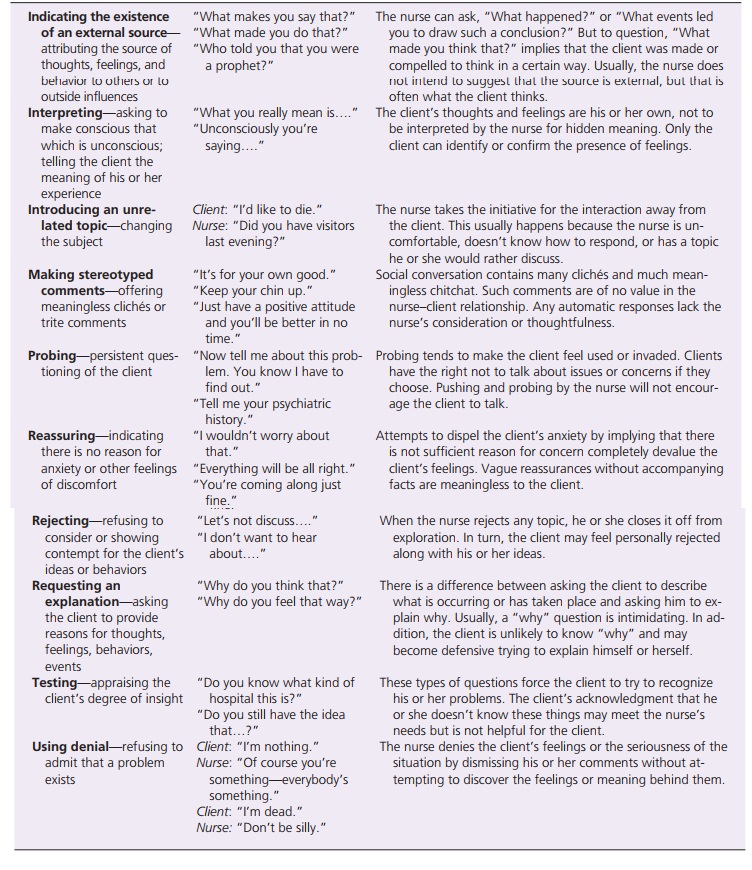
Avoiding Nontherapeutic Communication
In contrast, there are many nontherapeutic techniques that nurses
should avoid (Table 6.2). These responses cut off communication and make it
more difficult for the inter-action to continue. Responses such as “Everything
will work out” or “Maybe tomorrow will be a better day” may be intended to
comfort the client, but instead may impede the communication process. Asking
“why” questions (in an effort to gain information) may be perceived as criti-cism
by the client, conveying a negative judgment from the nurse. Many of these
responses are common in social interaction. Therefore, it takes practice for
the nurse to avoid making these types of comments.
![]()
![]()
Interpreting Signals or Cues
To understand what a client means, the nurse watches and listens
carefully for cues. Cues (overt and
covert) are ver-bal or nonverbal messages that signal key words or issues
for the client. Finding cues is a function of active listening. Cues can be
buried in what a client says or can be acted out in the process of
communication. Often, cue words introduced by the client can help the nurse to
know what to ask next or how to respond to the client. The nurse builds his or
her responses on these cue words or con-cepts. Understanding this can relieve
pressure on students who are worried and anxious about what question to ask
next. The following example illustrates questions the nurse might ask when responding
to a client’s cue:
Client: “I had a boyfriend when I was younger.”
Nurse: “You had a boyfriend?” (reflecting) “Tell me about you and your boyfriend.”(encouraging
description)
“How old were
you when you had this boy-friend?” (placing events in time or
sequence)
If a client has difficulty attending to a conversation and drifts
into a rambling discussion or a flight of ideas, the nurse listens carefully
for a theme or a topic around which the client composes his or her words. Using
the theme, the nurse can assess the nonverbal behaviors that accompany the
client’s words and build responses based on these cues. In the following
examples, the underlined words are themes and cues to help the nurse formulate
further communication.
Theme of sadness:
Client: “Oh, hi, nurse.” (face is sad; eyes look teary; voice is
low, with little inflection)
Nurse: “You seem sad today, Mrs. Venezia.”
Client: “Yes, it is the anniversary of my husband’s death.”
Nurse: “How long ago did your husband die?” (Or the nurse can use the
other cue.)
Nurse: “Tell me about your husband’s death, Mrs. Venezia.”
Theme of loss of control:
Client: “I had a fender bender this morning. I’m okay. I lost my wallet, and I have to go to the bank
to cover a check I wrote last night. I can’t get in contact with my husband at
work. I don’t know where to start.”
Nurse: “I sense you feel out of control” (translating into feelings).
Clients may use many word patterns to cue the listener to their
intent. Overt cues are clear, direct
statements of intent, such as “I want to die.” The message is clear that the
client is thinking of suicide or self-harm. Covert cues are vague or indirect messages that need
interpretationand exploration—for example, if a client says, “Nothing can help
me.” The nurse is unsure, but it sounds as if the client might be saying he
feels so hopeless and helpless that he plans to commit suicide. The nurse can
explore this covert cue to clarify the client’s intent and to protect the
client. Most suicidal people are ambivalent about whether to live or die and
often admit their plan when directly asked about it. When the nurse suspects
self-harm or suicide, he or she uses a yes/no question to elicit a clear
response.
Theme of hopelessness and suicidal ideation:
Client: “Life is hard. I want it to be done. There is no rest. Sleep, sleep is good . . . forever.”
Nurse: “I hear you saying things seem hope-less. I wonder if you are
planning to kill your-self” (verbalizing the implied).
Other word patterns that need further clarification for meaning
include metaphors, proverbs, and clichés. When a client uses these figures of
speech, the nurse must follow up with questions to clarify what the client is
trying to say.
A metaphor is a phrase that describes an object or a situation by
comparing it to something else familiar.
Client: “My son’s bedroom looks like a bomb went off.”
Nurse: “You’re saying your son is not very neat” (verbalizing the implied).
Client: “My mind is like mashed potatoes.”
Nurse: “I sense you find it difficult to put thoughts together” (translating
into feelings).
Proverbs are old accepted sayings with generally accepted meanings.
Client: “People who live in glass houses shouldn’t throw stones.”
Nurse: “Who do you believe is criticizing you but actually has similar problems?” (encourag-ing
description of perception)
A cliché is an expression that has become trite and gen-erally
conveys a stereotype. For example, if a client says, “she has more guts than
brains,” the implication is that the speaker believes the woman to whom he or
she refers is not smart, acts before thinking, or has no common sense. The
nurse can clarify what the client means by saying, “Give me one example of how
you see Mary as having more guts than brains” (focusing).
Related Topics