Chapter: Obstetrics and Gynecology: Premenstrual Syndromeand Premenstrual Dysphoric Disorder
Symptoms of Premenstrual Syndrome and Premenstrual Dysphoric Disorder
SYMPTOMS
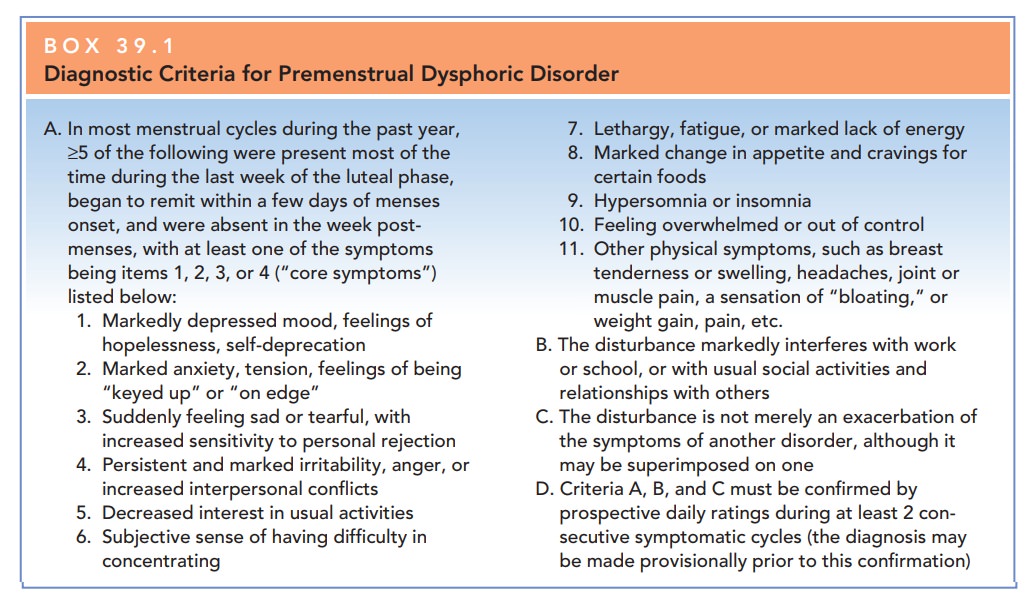
Over 200 symptoms have been attributed to PMS. Each patient presents with her own constellation of symptoms, thus making specific symptoms less important than the cyclic occurrence of the symptoms. Somatic symptoms that are most common include abdominal bloating and fatigue. Other symptoms include breast swelling and pain (masto-dynia), headache, acne, digestive upset, dizziness, sensitiv-ity to external stimuli, and hot flushes. The most common behavioral symptom is emotional lability. Other behavioral symptoms include irritability, depressed mood, anxiety, hostility, lachrymosity, increased appetite, difficulty con-centrating, and changes in libido. Box 39.1 presents the diagnostic criteria for PMDD as described in the DSM-IV. Box 39.2 lists the diagnostic criteria for PMS. The criteria for the diagnosis of PMDD are more rigorous than those of PMS and emphasize the existence of mood-related symp-toms. PMS can be diagnosed on the basis of either mood or physical symptoms.
Etiology
Many theories have been proposed to explain PMS, includ-ing altered levels of estrogen, progesterone, endorphins, cat-echolamines, vitamins, and minerals, but none provides a single, unified explanation that accounts for all the variations that are seen.
No compelling variations in any
of these substances have been found in women who have symptoms, compared to
women without symptoms, with the exception of some pre-liminary studies on serotonin.
Although it has been pro-posed that a low luteal-phase progesterone level is
the cause of what is now recognized as PMS or PMDD, measurement of serum
progesterone values and clinical results of proges-terone supplementation have
not supported this theory.
Currently
the data support a theory of serotoninergicdysregulation
as the basis for PMS/PMDD.Normal cyclichormonal
fluctuations can trigger an abnormal serotonin response. Monoamine oxidase
reduces serotonin availabil-ity, progesterone potentiates monoamine oxidase,
and estro-gen potentiates monoamine oxidase inhibitors. Thus, the availability
of serotonin is decreased in the progesterone-dominant luteal phase. However,
the interaction must be more complex, because replacement of progesterone alone
does not ameliorate PMS symptoms. Absolute levels of progesterone have not been
found to be different in women with PMS and those without, and monoamine
oxidase inhibitors do not improve symptoms in these patients. More recent data
implicates γ-aminobutyric
acid (GABA) as an important factor in decreasing levels of allopregnanolone, a
progesterone metabolite.
Diagnosis
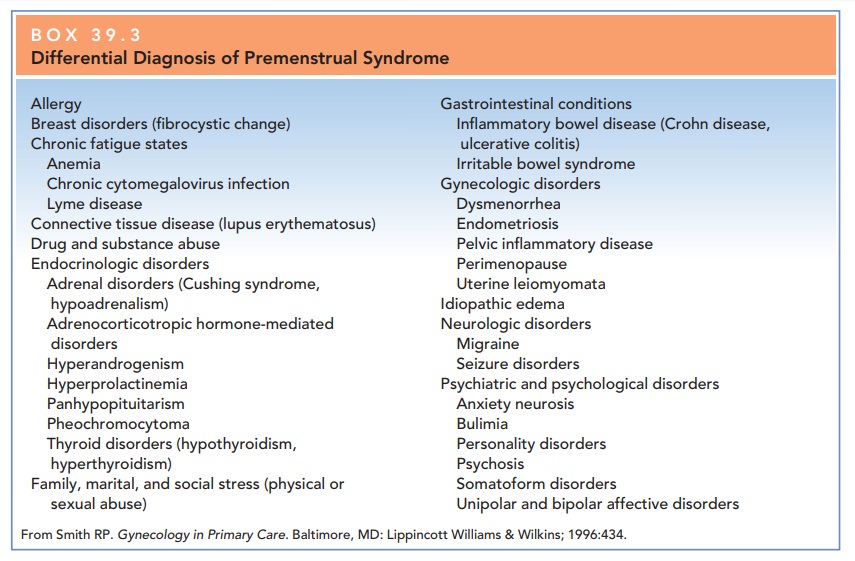
Virtually any condition that
results in mood or physical changes in any cyclic fashion may be included in
the dif-ferential diagnosis of PMS (Box 39.3). Studies have shown that a
patient’s recall of symptoms and timing of symp-toms is often biased and thus
inaccurate, because of wide-spread societal expectations and cultural
prominence of “the premenstrual syndrome.” The
majority of patients whopresent for treatment of PMS do not actually
demonstrate symp-toms restricted to the luteal phase.
The
diagnosis of PMS and PMDD can be very subjective and thus should be rigorously
established using the criteria outlined.
The physician must remain open-minded
at the outset, and not prematurely exclude the primary problem. In the
differential diagnosis, the physician should consider med-ical problems,
psychiatric disorders, and premenstrual exacerbations of medical and/or
psychiatric conditions: Perimenopause can also present with similar symptoms.
Because the etiology of PMS and
PMDD is not clear, no definitive historical, physical examination, or
labora-tory markers are available to aid in diagnosis. At present,the diagnosis of PMS and PMDD is based on documentation of
the relationship of the patient’s symptoms to the luteal phase.
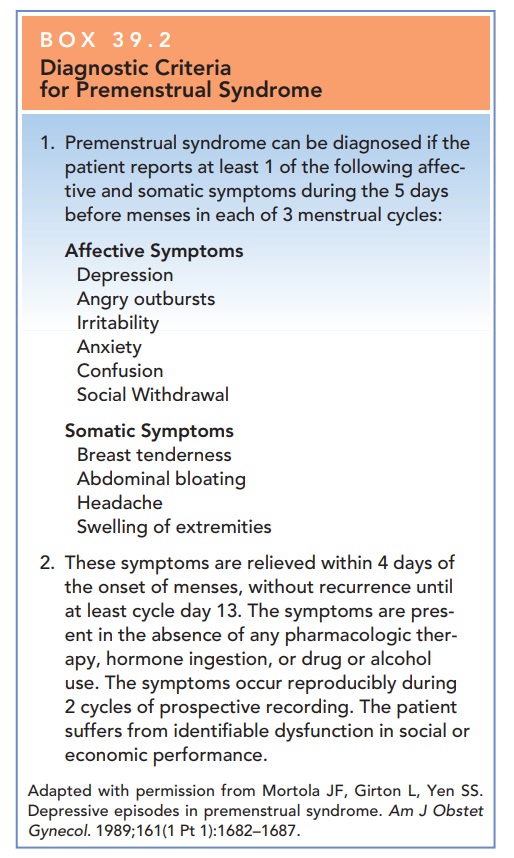
Box 39.2
Diagnostic Criteria for Premenstrual Syndrome
Premenstrual syndrome can be diagnosed if the patient reports at least 1
of the following affec-tive and somatic symptoms during the 5 days before
menses in each of 3 menstrual cycles:
Affective
Symptoms
Depression
Angry outbursts Irritability Anxiety Confusion Social Withdrawal
Somatic
Symptoms
Breast
tenderness Abdominal bloating Headache
Swelling
of extremities
These symptoms are relieved within 4 days of the onset of menses, without recurrence until at least cycle day 13. The symptoms are pres-ent in the absence of any pharmacologic ther-apy, hormone ingestion, or drug or alcohol use. The symptoms occur reproducibly during 2 cycles of prospective recording. The patient suffers from identifiable dysfunction in social or economic performance.
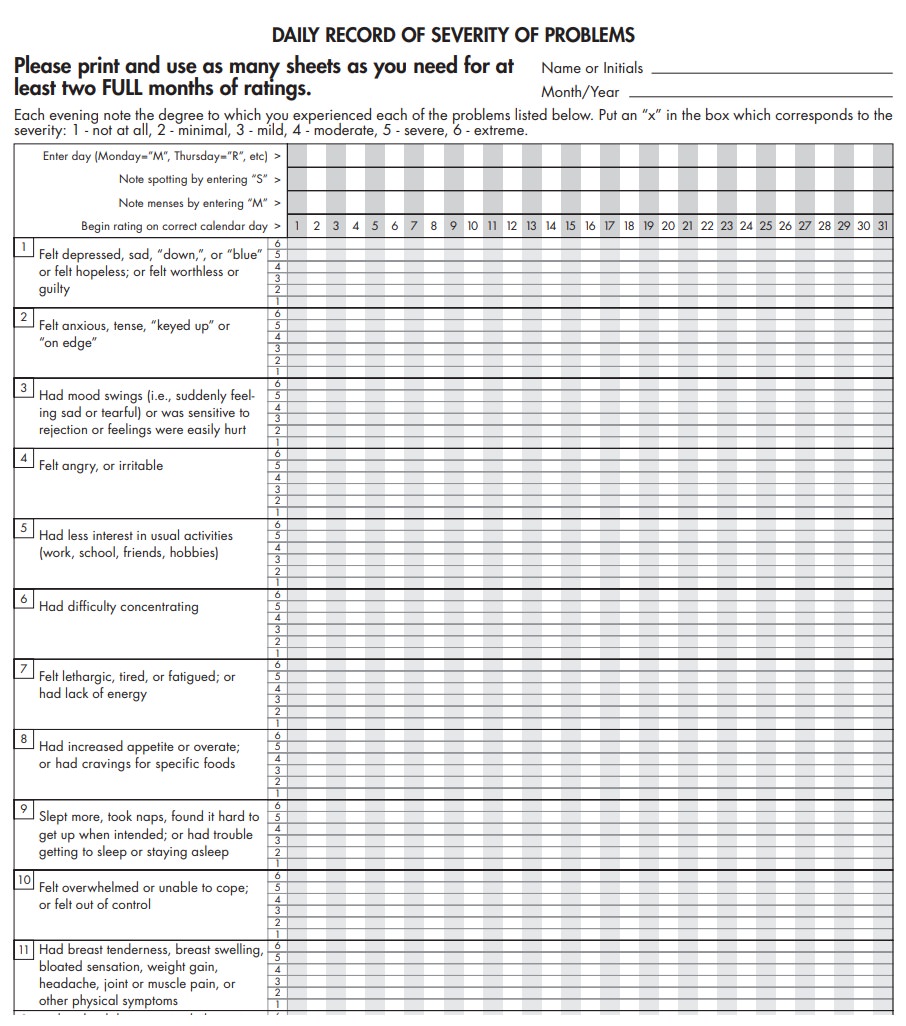
Prospective documentation of
symptoms can be accom plished using a menstrual
diary in two or more consec-utive menstrual cycles. The patient is asked to
monitor her symptoms and the pattern of menstrual bleeding for 2 or more
cycles. For PMS, she needs only to have one of the listed symptoms, but must
have a symptom-free period. For PMDD, the patient is asked to also monitor the
severity of symptoms. She must demonstrate 5 of the listed 11 symptoms (see Box
39.2), one of which must be a core symptom. She also must demonstrate a
symptom-free follicular phase. If her symptoms persist during the follicular
phase but are less severe, one must consider luteal phase worsening of a
different disorder (sometimes called entrainment).
Many
physical and psychiatric disorders are known to worsen in the luteal phase,
including irritable bowel syndrome and major depressive disorder.
It is important to distinguish
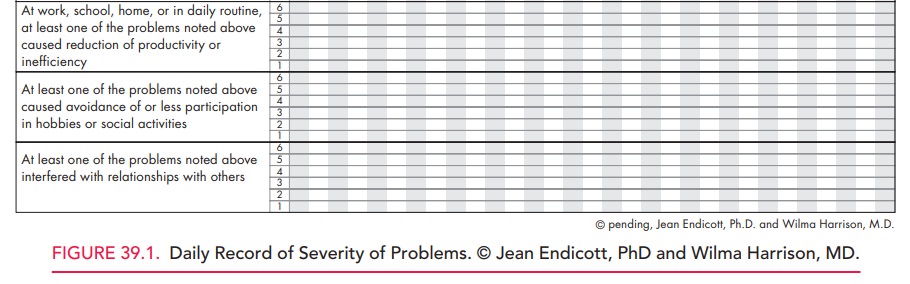
these disorders from PMDD. A variety of diagnostic tools exist to assist patients
with keeping their menstrual diaries. Figure 39.1 shows one such tool called
“Daily Record of Severity of Problems.”
Patients
with PMS should be evaluated to rule out specific pathology, although it is
also important to understand that no specific physical findings are diagnostic
of PMS.
It is reasonable to perform a
complete blood count and evaluate the thyroid-stimulating hormone (TSH) level,
because thyroid disease and anemia are quite common in young menstruating
women; however, there is no evidence that anemia or thyroid disease occur more
frequently in patients who present for treatment of PMS or PMDD.
Related Topics