Chapter: Essentials of Psychiatry: Substance Abuse: Phencycline Use Disorders
Substance Abuse: Phencycline Use Disorders
Substance Abuse: Phencycline Use Disorders
Phencyclidine (PCP) failed its development as a
potential general anesthetic agent during the 1950s because of its propensity
to cause psychotic episodes during emergence that were sometimes severe and
violent, and lasted from hours to days. PCP psychosis closely resembles
schizophrenia in terms of symptoms, signs and thought disorder. A single very
small dose of PCP given to a normal sub-ject induces a psychotic state lasting
for several hours, while in a person with schizophernia, the psychosis can be exacerbated
for several weeks by the fact that it is easy to synthesize. Many users
consumed PCP on a daily or near-daily basis for weeks or months at a time.
There were numerous instances of severe medical toxicity, a number of deaths
from overdoses, and many cases of prolonged (up to six weeks) psychoses in
users without preexisting psychotic disorders. In addition to CNS effects, PCP
overdose involves sym-pathomimetic, neuromuscular and renal effects that can
result in tis-sue damage and death. These problems are compounded by PCP’s
lipophilicity, long half-life and still longer duration of action. The
incidence and prevalence of PCP abuse have declined markedly since the late
1970s to early 1980s; however, PCP abuse continues and remains relatively high
in certain areas of the USA. PCP exerts its characteristic effects by
noncompetitive blockade of the N-me-thyl D-aspartate class of glutamate
receptors. Ketmine is a PCP de-rivative that shares PCP’s mechanism of action
and is approved for general effects are less frequent and severe owing to the
lower po-tency and shorter duration of ketamine action compared with PCP.
Epidemiology
As of the year 2000, the highest rates of PCP use
during the previous year were observed among 18- to 20-year-olds, followed by 12-
to 17-, 21- to 25-, and 26- to 34-year-olds. In 2000, among Americans aged 12
or older, it was estimated that 54 000 had used PCP within the previous month,
264 000 within the previous year and 5 693 000 (2% of the population) within
their lifetimes (Substance Abuse and Mental Health Services Administration,
2001). In the same year, PCP ranked 31st among the top 50 drugs mentioned most
frequently in drug-related emergency department episodes nationwide show-ing a
48% increase in ER mentions compared with 1999 (Substance Abuse and Mental
Health Services Administration, 2002).
In 1983, more than 66% of PCP-related deaths
reported to the Drug Abuse Warning Network involved at least another one drug.
Many of the PCP-related deaths were not the result of overdose or drug
interaction or reaction, but the direct result of some external
event facilitated by intoxication (e.g., homicides,
accidents). The various manners of death (such as drowning and being shot by
police) reported are consistent with the disorientation and violent aggressive
behavior that can be stimulated by PCP (Crider, 1986).
Etiology and Pathophysiology
The effects of low-dose PCP administration have
been extensively studied in volunteers. In normal subjects single intravenous
doses of 0.05 to 0.1 mg/kg induced withdrawal, negativism and in some cases
catatonic posturing; thinking processes became concrete, idiosyn-cratic and
bizarre in the absence of significant physical or neurologi-cal findings; and
drug effects persisted for 4 to 6 hours In contrast to lysergic acid
diethylamide (LSD) or amphetamine PCP was noted to induce disturbances in
symbolic thinking perception and attention strikingly similar to those observed
in schizophrenia. Administra-tion of PCP to schizophrenic subjects caused
exacerbation of ill-ness-specific symptoms persisting up to several weeks,
suggesting that schizophrenic or preschizophrenic individuals may be at
sig-nificantly increased risk of behavioral effects from PCP abuse.
Phenomenology and Variations in Presentation
Physicians must be alert to the wide spectrum of
PCP effects on multiple organ systems. Because fluctuations in serum levels may
occur unpredictably, a patient being treated for apparently selective
psychiatric or behavioral complications of PCP abuse may suddenly undergo
radical alterations in medical status; emergency medi-cal intervention may
become necessary to avoid permanent organ damage or death. Any patient
manifesting significant cardiovascu-lar, respiratory, neurological, or
metabolic derangement subsequent to PCP use should be evaluated and treated in
a medical service; the psychiatrist plays a secondary role in diagnosis and
treatment until physiological stability has been reached and sustained.
PCP-intoxicated patients may come to medical
attention on the basis of alterations in mental status; bizarre or violent
be-havior; injuries sustained while intoxicated; or medical complica-tions,
such as rhabdomyolysis, hyperthermia, or seizures (Bald-ridge and Bessen,
1990). As illicit ketamine use has increased significantly as part of the “club
drug” phenomenon, it is impor-tant to remember that ketamine can induce the
same spectrum of effects and complications, the chief difference from PCP being
the much shorter duration of action of ketamine.
Studies of normal volunteers suggested that the
acute psy-chosis induced by a single low dose of PCP usually lasts for 4 to 6
hours (Javitt and Zukin, 1991). However, in some PCP users psy-chotic symptoms
including hallucinations, delusions, paranoia, thought disorder and catatonia,
with intact consciousness, have been reported to persist from days to weeks
after single doses. Sudden and impulsive violent and assaultive behaviors have
been reported in PCP-intoxicated patients without previous histories of such
conduct.
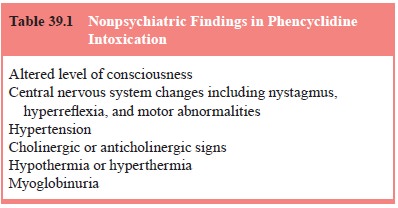
In PCP intoxication, the central nervous, cardiovascular, respiratory and peripheral autonomic systems are affected to de-grees ranging from mild to catastrophic (Table 39.1). The level of consciousness may vary from full alertness to coma. Coma of variable duration may occur spontaneously or after an episode of bizarre or violent behavior Nystagmus (which may be horizontal, vertical, or rota-tory) has been described in 57% of a series of 1 000 patients (McCarron et al., 1981). Consequences of PCP-induced central nervous system hyperexcitability may range from mildly in-creased deep tendon reflexes to grand mal seizures (observed in 31 of a series of 1 000 PCP-intoxicated patients) or status epilep-ticus (McCarron et al., 1981; Kessler et al., 1974). Seizures are usually generalized, but focal seizures or neurological deficits have been reported, probably on the basis of focal cerebral vaso-constriction (Crosley and Binet, 1979). Other motor signs have been observed, such as generalized rigidity, localized dystonias, facial grimacing and athetosis.
Hypertension, one of the most frequent physical
findings, was described in 57% of 1 000 patients evaluated, and it was found to
be usually mild and self-limiting, but 4% had severe hypertension, and some
remained hypertensive for days (McCarron et
al., 1981). Tachycardia occurs in 30% of patients. PCP-induced tachypnea can progress to periodic
breathing and respiratory arrest (Hurlbut, 1991). Autonomic signs seen in PCP
intoxication may be cholinergic (diaphoresis, bronchospasm, miosis, salivation,
bronchorrhea) or anticholinergic (mydriasis, urinary retention). Hypothermia
and hyperthermia have been observed (McCarron et al., 1981). Hyperthermia may reach malignant proportions (Thompson, 1979). Rhabdomyolysis
frequently results from a combination of PCP-induced muscle contractions and
trauma occurring in relation to injuries sustained as a result of behavioral
effects. Acute renal failure can result from myoglobinuria.
Assessment
Special Issues in Psychiatric Examination and History
The disruption of normal cognitive and memory
function by PCP frequently renders patients unable to give an accurate history.
Therefore, assay of urine or blood for drugs may be the only way to establish
the diagnosis. PCP is frequently taken in forms in which it has been used to
adulterate other drugs, such as mari-juana and cocaine, often without the
user’s knowledge. One of the most recent and alarming manifestations of this
phenomenon is a preparation known variously as “illy”, “hydro”, “wet”, or
“fry”, consisting of a marijuana cigarette or blunt containing
formalde-hyde/formalin (which is advertised) and PCP (which often is not). By
disrupting sensory pathways, PCP frequently renders users hypersensitive to
environmental stimuli to the extent that physi-cal examination or psychiatric
interview may cause severe agita-tion. If PCP intoxication is suspected,
measures should be taken from the outset to minimize sensory input. The patient
should be evaluated in a quiet, darkened room with the minimal necessary number
of medical staff present. Assessments may need to be interrupted periodically.
Relevant Physical Examination and Laboratory Findings
Vital signs should be obtained immediately on presentation.
Temperature, blood pressure and respiratory rate are dose-dependently increased
by PCP and may be of a magnitude requiring emergency medical treatment to avoid
the potentially fatal complications of malignant hyperthermia, hypertensive
cri-sis and respiratory arrest. In all cases, monitoring of vital signs should
continue at 2- to 4-hour intervals throughout treatment, because serum PCP
levels may increase spontaneously as a re-sult of mobilization of drug from
lipid stores or enterohepatic recirculation. Analgesic and behavioral changes
induced by PCP not only predispose patients to physical injury but also mask
these injuries, which may be found only with careful physical examination.
Because PCP is usually supplied in combination with
other drugs and is often misrepresented, toxicological analysis of urine or
blood is essential. However there may be circumstances in which PCP may not be
detected in urine even if it is present in the body, for example, when the
urine is alkaline. On the other hand, in chronic PCP users, drug may be
detected in urine up to 30 days after last use (Simpson et al., 1982–1983). It must be kept in mind that false-positive PCP
results can be caused by the presence of venlafaxine and O-desmethylvenlafaxine (Sena et
al., 2002), or dextromethorphan (Shier, 2000). Urine should be tested for
heme because of the possible complication of myoglobinuria.
Differential Diagnosis
The presence of nystagmus and hypertension with
mental status changes should raise the possibility of PCP intoxication. Because
of the close resemblance of both the acute and the prolonged forms of PCP
psychosis to schizophrenia, and the increased sen-sitivity of patients with
schizophrenia to the psychotomimetic ef-fects of the drug, an underlying
schizophrenia spectrum disorder should be considered, particularly if paranoia
or thought disorder persists beyond 4 to 6 weeks after last use of PCP. PCP
psycho-sis may also resemble mania or other mood disorders. Robust response of
psychotic symptoms to treatment with neuroleptics would favor a diagnosis other
than simple PCP psychosis.
PCP psychosis is readily distinguishable from LSD
psy-chosis in normal as well as in individuals with schizophrenia by the lack
of typical LSD effects, such as synesthesia. In cases involving prominent
PCP-induced neurological, cardiovascular, or metabolic derangement,
encephalitis, head injury, postictal state and primary metabolic disorders must
be ruled out. Either intoxication with or withdrawal from sedative–hypnotics
may be associated with nystagmus. Neuroleptic malignan at syndrome should be
ruled out in the differential diagnosis of PCP-induced hyperthermia and muscle
rigidity.
Course and Natural History
As drug levels decline, the clinical picture
recedes in five to 21 days through periods of moderating neurological,
autonomic and metabolic impairments to a stage at which only psychiatric
impairments are apparent. Once the physical symptoms and signs have cleared the
period of simple PCP psychosis may last 1 day to 6 weeks, whether or not
neuroleptics are administered, during which the psychiatric symptoms and signs
abate gradually and progressively. Even after complete recovery flashbacks may
oc-cur if PCP sequestered in lipid stores is mobilized. Any underly-ing
psychiatric disorders can be detected and evaluated only after complete
resolution of the drug-induced psychosis.
Overall Goals of Treatment
The hierarchy of treatment goals begins with
detection and treatment of physical manifestations of PCP intoxication. Equally
important are measures to anticipate PCP-induced impulsive, violent behaviors
and provide appropriate protec-tion for the patient and others. The patient
must then be closely observed during the period of PCP-induced psychosis, which
may persist for weeks after resolution of physical symptoms and signs. Finally,
the possibly dramatic medical and psychiat-ric presentation and its resolution
must not divert the attention of the psychiatrist from full assessment and
treatment of the patient’s drug-seeking behavior.
Physician–Patient Relationship in Psychiatric Management
In contrast to psychotic states induced by drugs
such as LSD, in which “talking the patient down” (by actively distracting the
pa-tient from his LSD-induced sensory distortions and convincing the patient
that his or her distress stems from nothing more than the temporary effects of
a drug that soon will wear off) may be highly effective, no such effort should
be made in the case of PCP psychosis, particularly during the period of acute
intoxication, because of the risk of sensory overload that can lead to
dramati-cally increased agitation. The risk of sudden and unpredictable
impulsive, violent behavior can also be increased by sensory stimulation.
Pharmacotherapy and Somatic Treatments
There is no pharmacological competitive antagonist
for PCP. Oral or intramuscular benzodiazepines are recommended for agitation.
Neuroleptics usually have little or no effect on acute or chronic PCP-induced
psychosis or thought disorder. Because they lower the seizure threshold,
neuroleptics should be used with caution. Physical restraint may be lifesaving
if the patient’s behavior poses an imminent threat to his or her safety or that
of others; however, such restraint risks triggering or worsening
rhabodomyolysis.
Related Topics