Chapter: Human Neuroanatomy(Fundamental and Clinical): The Spinal Cord : Gross Anatomy and Some features of Internal Structure
Spinal Nerves & Spinal Segments
Spinal Nerves & Spinal Segments
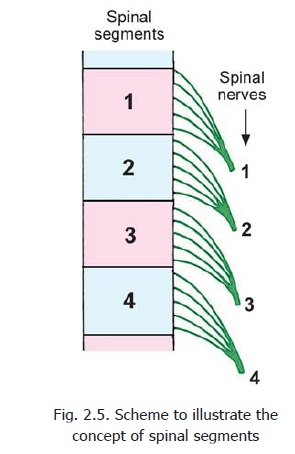
The spinal cord gives attachment, on either side, to a series of spinal nerves. Each spinal nerve arises by two roots, anterior (or ventral) and posterior (or dorsal) (Fig. 2.4). Each root is formed by aggregation of a number of rootlets that arise from the cord over a certain length (Fig. 2.5). Thelength of the spinal cord giving origin to the rootlets of one spinal nerve constitutes one spinal segment.However, this definition applies only to the superficial attachment of nerve roots. The neurons associated with one spinal nerve extend well beyond the confines of a spinal segment.
The spinal cord is made up of thirty one segments: 8 cervical, 12 thoracic, 5 lumbar, 5 sacral and one coccygeal.
Note that in the cervical and coccygeal regions the number of spinal segments, and of spinal nerves, does not correspond to the number of vertebrae.
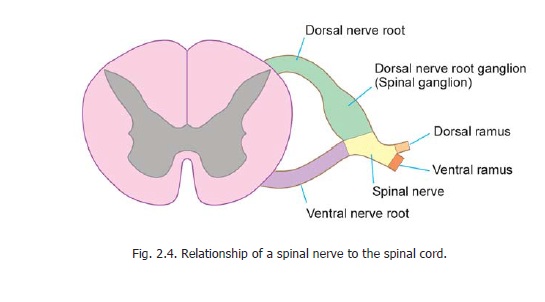
The rootlets that make up the dorsal nerve roots are attached to the surface of the spinal cord along a vertical groove (called thepostero-lateral sulcus) opposite the tip of the posterior grey column (Fig. 2.4). The rootlets of the ventral nerve roots are attached to the anterolateral aspect of the cord opposite the anterior grey column. The ventral and dorsal nerve roots join each other to form a spinal nerve. Just proximal to the junction of the two roots the dorsal root is marked by a swelling called the dorsalnerve root ganglion, or spinal ganglion (Fig. 2.4).
Development
In early fetal life (third month) the spinal cord is as long as the vertebral canal, and each spinal nerve arises from the cord at the level of the corresponding intervertebral foramen. In subsequent development the spinal cord does not grow as much as the vertebral column and its lower end, therefore, gradually ascends to reach the level of the third lumbar vertebra at the time of birth, and to the lower border of the first lumbar vertebra in the adult.
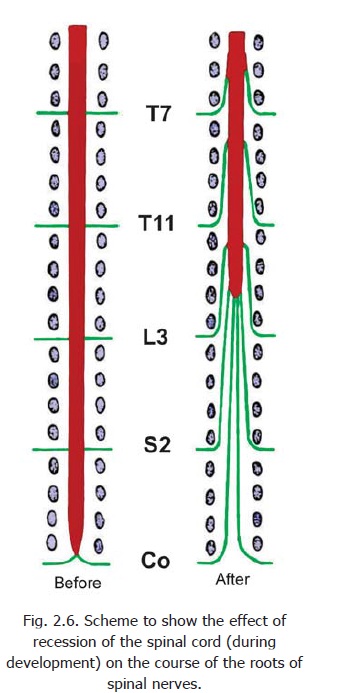
As a result of this upward migration of the cord the roots of spinal nerves have to follow an oblique downward course to reach the appropriate intervertebral foramen (Fig. 2.6). This also makes the roots longer. The obliquity and length of the roots is most marked in the lower nerves and many of these roots occupy the vertebral canal below the level of the spinal cord. These roots constitute the cauda equina.
Clinical:
Another result of the upward recession of the spinal cord is that the spinal segments do not lie opposite the corresponding vertebrae. This fact is clinically important. For estimating the position of a spinal segment in relation to the surface of the body it is important to remember that a vertebral spine is always lower than the corresponding spinal segment. As a rough guide it may be stated that in the cervical region there is a difference of one segment (e.g., the 5th cervical spine overlies the 6th cervical segment); in the upper thoracic region there is a difference of two segments (e.g., the 4th thoracic spine overlies the 6th thoracic segment); and in the lower thoracic region there is a difference of three segments (e.g., the 9th thoracic spine lies opposite the 12th thoracic segment).
Basic:
The spinal cord is not of uniform thickness. The spinal segments that contribute to the nerves of the upper limbs are enlarged to form the cervical enlargement of the cord. Similarly, the segments innervating the lower limbs forms the lumbar enlargement (Fig. 2.2).
In addition to spinal nerves the upper five or six cervical segments of the spinal cord give origin to a series of rootlets that emerge on the lateral aspect (midway between the anterior and posterior nerve roots of spinal nerves). These rootlets join to form the spinal root of the accessory nerve. This nerve travels upwards to enter the cranial cavity through the foramen magnum.
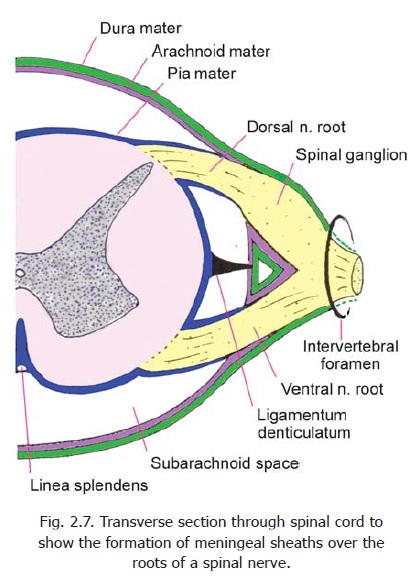
The spinal cord is surrounded by the meninges. These are the dura mater, the arachnoidmater, and the pia mater. The dura mater is a thick fibrous membrane. The arachnoid mater andpia mater are thin membranes. The space between the dura mater and the wall of the vertebral canal is called the extradural (or epidural) space, while the space between the dura andthe arachnoid is called thesubdural space. The arachnoid and pia are separated by the subarachnoid space which contains the cerebrospinal fluid (CSF) (Fig. 2.7).
The spinal dura mater forms a loose tubular covering for the spinal cord. We have seen that the spinal cord (and overlying pia mater) extends downwards only up to the lower border of the first lumbar vertebra. The dura and arachnoid (along with the subarachnoid space containing CSF), however extend up to the second sacral vertebra.
Between these two levels the subarachnoid space contains the spinal nerve roots forming the cauda equina.
In this region, a needle can be introduced into the subarachnoid space without danger of injury to the spinal cord. This procedure is called lumbar puncture (Fig. 2.2).
The dorsal and ventral roots of spinal nerves pass through the spinal dura mater separately. Sheaths derived from dura extend over the nerve roots. These dural sheaths reach up to the intervertebral foramina and are attached to the margins of these foramina. The dorsal and ventral nerve roots unite in the intervertebral foramina to form the trunks of spinal nerves. The pia mater and arachnoid mater also extend on to the roots of spinal nerves as sheaths. These sheaths reach up to the site where the nerve roots pass through dura mater (Fig. 2.7).
We have seen that below the level of the conus medullaris the spinal cord is continuous with the filum terminale. The filum terminale is made up mainly of pia mater. Below the level of the second sacral vertebra the filum terminale is surrounded by an extension of dura mater. It ends by gaining attachment to the dorsum of the first segment of the coccyx (Fig. 2.2).
Related Topics