Dietary Treatment, Dialysis Diet - Special Considerations for Clients with Renal Diseases | Nutrition and Diet Therapy: Diet and Renal Disease
Chapter: Nutrition and Diet Therapy: Diet and Renal Disease
Special Considerations for Clients with Renal Diseases
SPECIAL CONSIDERATIONS
FOR CLIENTS WITH RENAL DISEASES
Dietary Treatment of Renal Disease
Dietary treatment is
intended to slow the buildup of waste in the bloodstream. Decreasing waste in
the bloodstream will control symptoms of fluid retention, hyperkalemia, and
nausea and vomiting. The goal is to reduce the amount of excretory work
demanded of the kidneys while helping them maintain fluid, acid-base, and
electrolyte balance. Clients require sufficient protein to prevent malnutrition
and muscle wasting. Too much, however, can contribute to uremia. Typically, the
client with chronic renal failure will have protein and sodium, and possibly
potassium and phosphorus, restricted.
It is essential that
renal clients receive sufficient calories—25 to 50 calories per kilogram of
body weight—unless they are overweight. Energy requirements should be fulfilled
by carbohydrates and fat. The fats must be unsaturated to prevent or check
hyperlipidemia. If the energy requirement is not met by carbohydrates and fat,
ingested protein or body tissue will be metabolized for energy. Either would
increase the work of the kidneys because protein increases the amount of
nitrogen waste the kidneys must handle. The diet may limit protein to as little
as 40 grams for predialysis clients. The specific amount of protein allowed is
calculated according to the client’s glomerularfiltration
rate (GFR) and weight.
Fluids and sodium may
be limited to prevent edema, hypertension, and congestive heart failure.
Calcium supplements may be prescribed. In addition, vitamin D may be added and
phosphorus limited to prevent osteomalacia (softening of the bones due to
excessive loss of calcium). Phosphorus appears to be retained in clients with
kidney disorders, and a disproportionately high ratio of phosphorus to calcium
tends to increase calcium loss from bones.
Potassium may be
restricted in some clients because hyperkalemia tends to occur in end-stage renal disease (ESRD). Excess potassium can
cause cardiac arrest. Because of this danger, renal clients should not use salt
substi-tutes or low-sodium milk because the sodium in these products is
replaced with potassium. Potassium restriction can be especially difficult for
a renal client, who probably must limit sodium intake. Potassium is
particularly high infruits—one of the few foods a client on a sodium-restricted
diet may eat without concern.
Renal clients often
have an increased need for vitamins B, C, and D, and supplements are often
given. Vitamin A should not be given because the blood level of vitamin A tends
to be elevated in uremia. If a client is receiving antibiotics, a vitamin K
supplement may be given. Otherwise, supplements of vitamins E and K are not
necessary. Iron is commonly prescribed because anemia frequently develops in
renal clients. It is sometimes necessary to increase the amount of simple
carbohydrates and unsaturated fats to ensure sufficient calories.
Dialysis
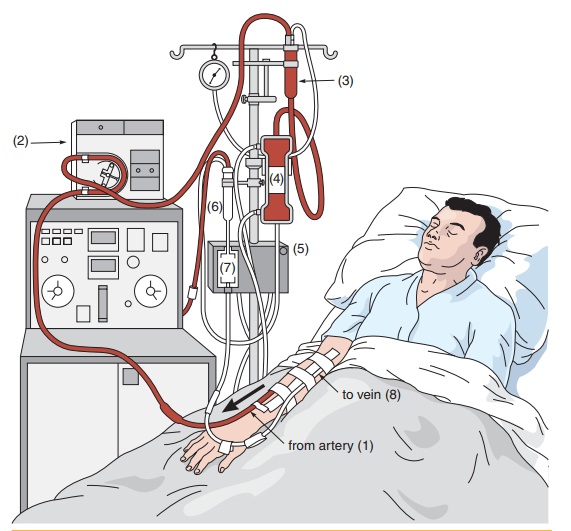
Dialysis is done by
either hemodialysis or peritoneal dialysis. The most common is
hemodialysis. Hemodialysis requires permanent access to the blood-stream
through a fistula. Fistulas are unusual openings between two organs. They are
often created near the wrist and connect an artery and a vein. Hemodialysis is
done three times a week for approximately 3 to 5 hours each visit (Figure
19-2).
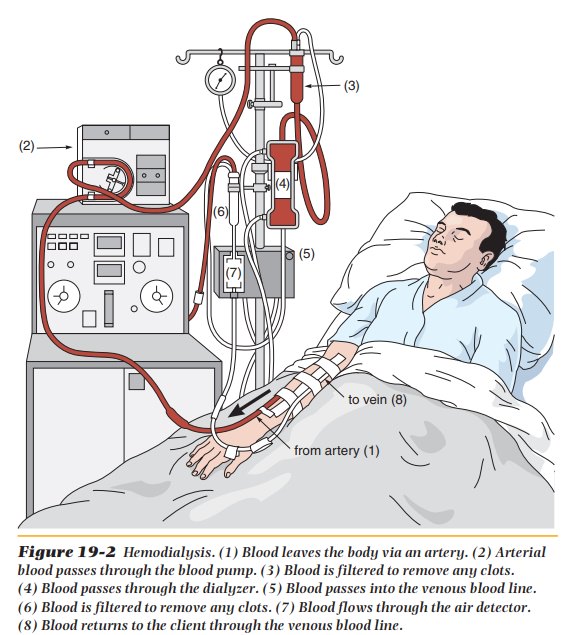
Peritoneal dialysis
uses the peritoneal cavity as a semipermeable membrane and is less efficient
than hemodialysis. Treatments usually last about 10 to 12 hours a day, three
times a week (Figure 19-3). Some clients also use continuous ambulatory
peritoneal dialysis (CAPD). The dialysis fluid is exchanged four or five times
daily, making this a 24-hour treatment. Clients on CAPD have a more normal
lifestyle than do clients on either hemodialysis or peritoneal dialysis. Some
complications associated with CAPD include peri-tonitis, hypotension, and
weight gain.
Diet during Dialysis
Dialysis
clients may need additional protein, but the amount must be carefully
controlled to prevent the accumulation of protein waste between treatments.
A
client on hemodialysis requires 1.0 to 1.2 grams of protein per kilo-gram of
body weight to make up for losses during dialysis. A client on peritoneal
dialysis will require 1.2 to 1.5 grams of protein per kilogram of body weight.
The protein needs for clients on CAPD are 1.2 grams per kilogram of body
weight. Seventy-five percent of this protein should be high biological value
(HBV) protein, which is found in eggs, meat, fish, poultry, milk, and cheese.
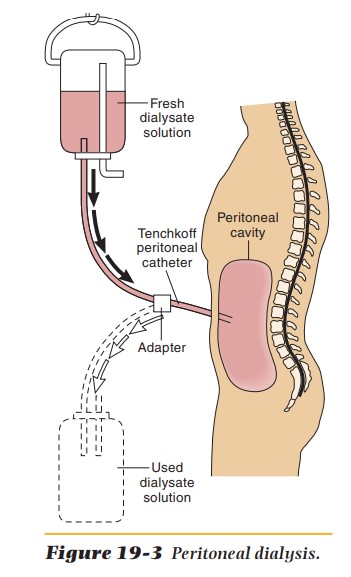
Potassium
is usually restricted for dialysis clients. Healthy people ingest from 2,000 to
6,000 mg per day. The daily intake allowed clients in renal failure is 3,000 to
4,000 mg. End-stage renal disease further reduces intake allowed to 1,500 to
2,500 mg a day. The physician will prescribe the milli-grams of potassium
needed by the client. Table 19-1 lists low-, medium-, and high-potassium fruits
and vegetables.
Clients
are taught to regulate their intake by making careful choices. Milk is normally
restricted to 1 ⁄2 cup a day because it is high in potassium and
high in methionine, an essential amino acid. A typical renal diet could be
written as “80-3-3,” which means 80 grams of protein, 3 grams of sodium, and 3
grams of potassium a day. There may be a phosphorus restriction also. And there
is often a need for supplements of water-soluble vitamins, vitamin D, calcium,
and iron.
The ability of the kidney to handle sodium and water in ESRD must be assessed often. Usually, the diet contains 3 grams of sodium, which is the equivalent of a no-added-salt diet. Sodium and fluid needs may increase with perspiration, vomiting, fever, and diarrhea. The fluid content of foods, other than liquids, is not counted in fluid restriction. Clients on fluid restriction must be taught to measure their fluid intake and urine output, examine their ankles for edema, and weigh themselves regularly.
Diet after Kidney Transplant
After kidney
transplant, there may be a need for extra protein or for the restric-tion of
protein. Carbohydrates and sodium may be restricted. The appropriate amounts of
these nutrients will depend largely on the medications given at that time.
Additional calcium and
phosphorus may be necessary if there was substantial bone loss before the
transplant. There may be an increase in appe-tite after transplants. Fats and
simple carbohydrates may be limited to prevent excessive weight gain.
Dietary Treatment of Renal Stones
Because the causes of
renal stones have not been confirmed, treatment of them may vary. In general,
however, large amounts of fluid—at least half of it water—are helpful in
diluting the urine, as is a well-balanced diet. Once the stones have been
analyzed, specific diet modifications may be indicated.
Calcium Oxalate Stones.About 80% of the
renal stones formedcontain calcium oxalate. Recent studies provide no support
for the theory that a diet low in calcium can reduce the risk of calcium
oxalate renal stones. In fact, higher dietary calcium intake may decrease the
incidence of renal stones for most people. Dietary intake of excessive animal
protein has been shown to be a risk factor for stone formation in some clients.
Stones containing
oxalate are thought to be partially caused by a diet especially rich in
oxalate, which is found in beets, wheat bran, chocolate, tea, rhubarb,
strawberries, and spinach. Evidence also indicates that deficiencies of
pyridoxine, thiamine, and magnesium may contribute to the formation of oxalate
renal stones.
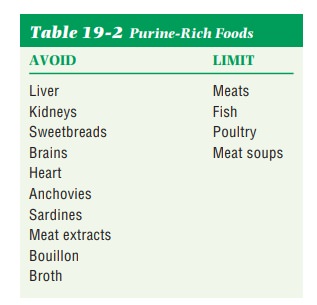
Uric Acid Stones.When the stones contain uric acid,
purine-richfoods are restricted (Table 19-2). Purines are the end products
of nucleopro-tein metabolism and are found in all meats, fish, and poultry.
Organ meats, anchovies, sardines, meat extracts, and broths are especially rich
sources of them. Uric acid stones are usually associated with gout, GI diseases
that cause diarrhea, and malignant disease.
Cystine Stones.Cystine is an amino acid. Cystine stones may
formwhen the cystine concentration in the urine becomes excessive because of a
hereditary metabolic disorder. The usual practice is to increase fluids and
recommend an alkaline-ash diet.
Struvite Stones.Struvite stones are composed of magnesium
ammo-nium phosphate. They are sometimes called infection stones because they
develop following urinary tract infections caused by certain microorganisms. A
low-phosphorus diet is often prescribed.
Related Topics