Chapter: Obstetrics and Gynecology: The Woman’s Health Examination
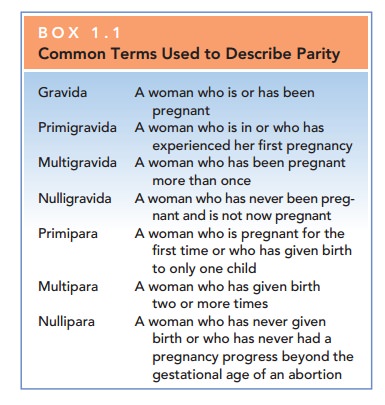
Review of Systems - Obstetrics and Gynecology
REVIEW OF SYSTEMS
Following the medical history, an
overall assessment of a patient’s health history on a system-by-system basis
should be conducted. This assessment provides an opportunity for a more focused
evaluation of the patient. This review should encompass all body systems (Box
1.2).
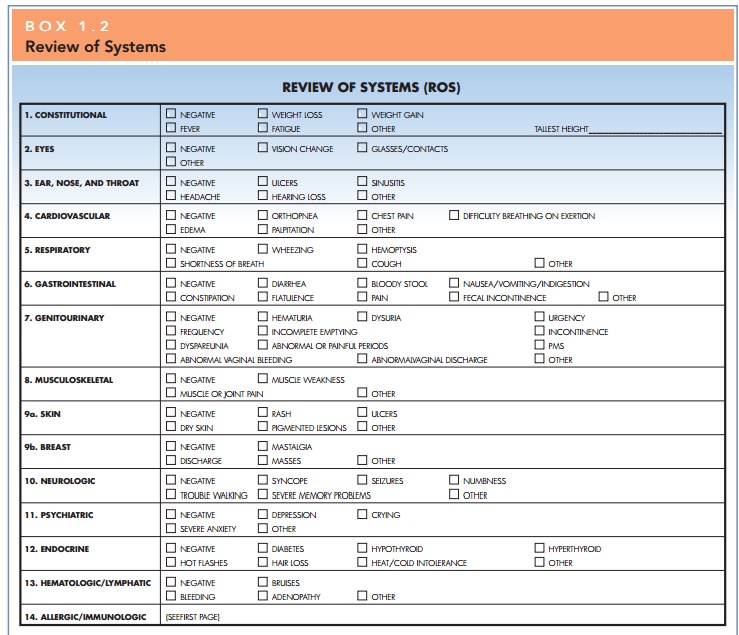
Physical Examination
The physical examination
encompasses an evaluation of a patient’s overall health as well as a breast and
gyneco-logic examination. The general
physical examination servesto detect abnormalities suggested by the medical
history as well as unsuspected problems. Specific information the
patientgives during the history should guide the practitioner to areas of
physical examination that may not be sur-veyed in a routine screening. The
extent of the exami-nation is based on the practitioner’s clinical relationship
with the patient, what is being medically managed by other clinicians, and what
is medically indicated. Areas that are included in this general examination are
listed in Box 1.3.
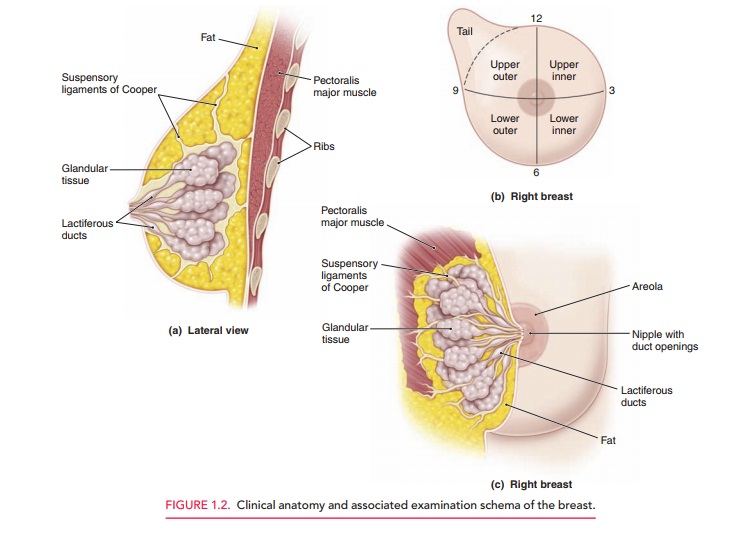
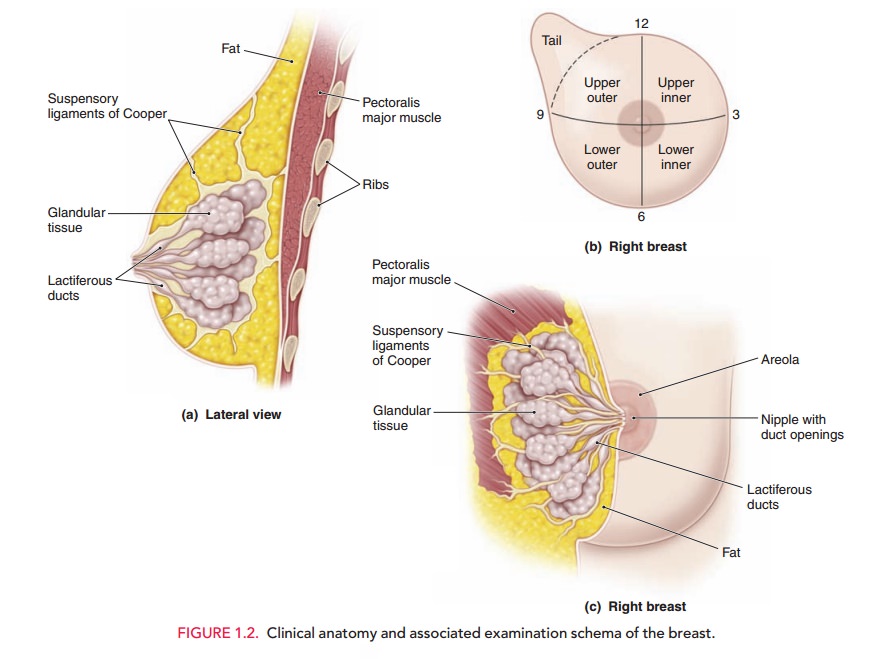
Breast Examination
The breast examination by a physician remains the best means of early
detection of breast cancer when combined with appropriately scheduled
mammography and regular breast self-examination (BSE). The results of the
breast examination may be expressed by description or diagram, or both, usually
with reference to the quadrants and tail region of the breast or by allusion to
the breast as a clock face with the nipple at the center (Fig. 1.2).
The breasts are first examined by inspection, with the patient’s arms at her sides, and then with her hands pressed against her hips, and/or with her arms raised over her head (Fig. 1.3). If the patient’s breasts are especially large and pendulous, she may be asked to lean forward so that the breasts hang free of the chest, facilitating inspec-tion.
Tumors often distort the relations of these
tissues, causing disruption of the shape, contour, or symmetry of the breast or
position of the nipple. Some asymmetry of the breasts is common, but marked
differences or recent changes deserve further evaluation.
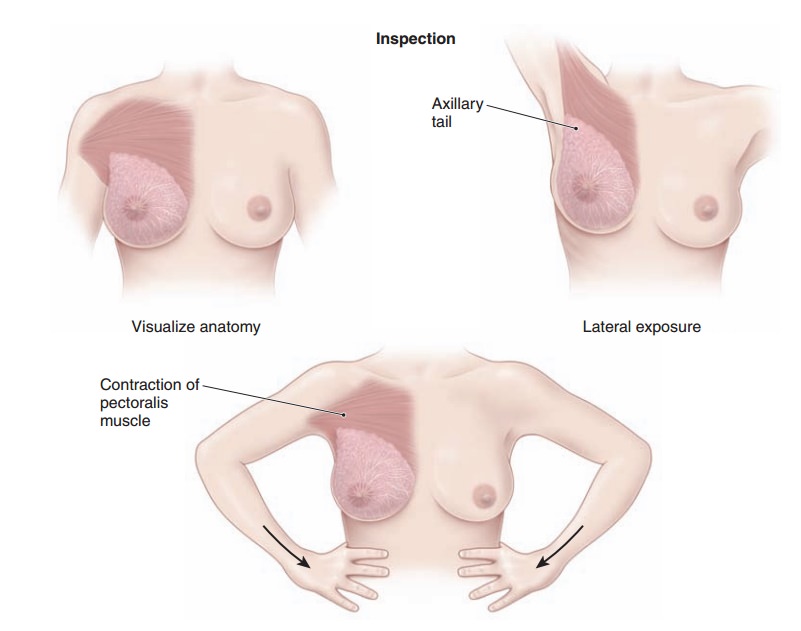
Discolorations or ulcerations of
the skin of the breast, areola, or nipple, or edema of the lymphatics that
causes a leathery puckered appearance of the skin (referred to as peaud’orange, or like the skin of an
orange), are abnormal. A clearor milky breast discharge is usually bilateral
and associated with stimulation or elevated prolactin levels (galactorrhea). Bloody discharge from
the breast is abnormal and usually unilateral; it usually does not represent
carcinoma, but rather inflammation of a breast structure. Evaluation is
nec-essary to exclude malignancy. Pus usually indicates infection, although an
underlying tumor may be encountered.
Very large breasts may pull
forward and downward, causing upper back pain and stooped shoulders. Disabling
pain and posture is usually considered sufficient for use of insurance coverage
for breast reduction
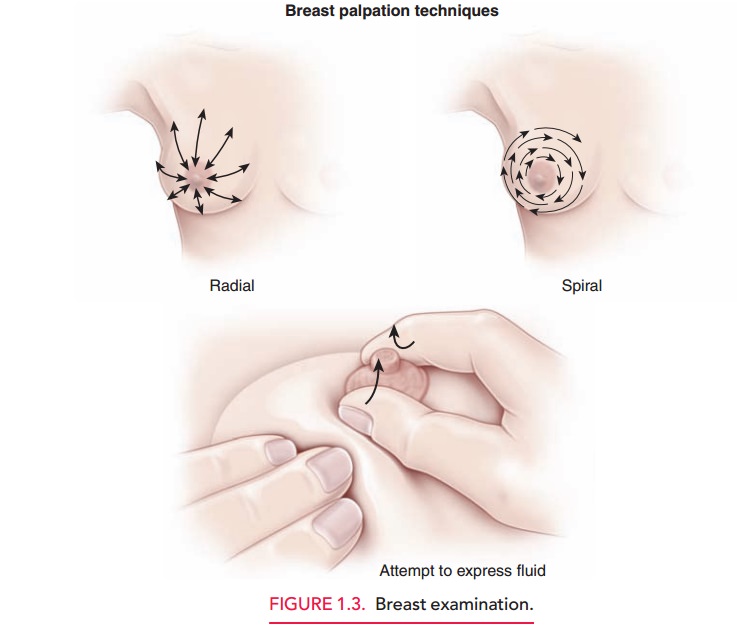
Palpation
follows inspection, first with the patient’sarms at
her sides and then with the arms raised over her head. This part of the
examination is usually done with the patient in the supine position. The
patient may also be seated, with her arm resting on the examiner’s shoulder or
over her head, for examination of the most lateral aspects of the axilla.
Palpation should be done with slow, careful maneuvers using the flat part of
the fingers and not the tips. The fingers are moved up and down in a wavelike
motion, moving the tissues under them back and forth, so that any breast masses
that are present can be more easily felt. The examiner should cover the entire
breast in a spi-ral or radial pattern, including the axillary tail. If masses
are found, their size, shape, consistency (soft, hard, firm, cystic), and mobility,
as well as their position, should be determined. Women with large breasts may
have a firm ridge of tissue located transversely along the lower edge of the
breast. This is the inframammary ridge, and is a nor-mal finding.
The examination is concluded with gentle pressure inward and then upward at the sides of the areola to express fluid. If fluid is noted on inspection or is expressed, it should be sent for culture and sensitivity and cytopath-ology (fixed in the same manner as for a slide-technique Pap test).
Pelvic Examination
Preparation for the pelvic
examination begins with the patient emptying her bladder. Everything that is
going to happen should be explained before it occurs. Follow-ing the precept
“Talk before you touch” avoids anything unexpected.
Abdominal and pelvic examinations
require relaxation of the muscles. Techniques that help the patient to relax
include encouraging the patient to breathe in through her nose and out through
her mouth, gently and regularly, rather than holding her breath, and helping
the patient to identify specific muscle groups (such as the abdominal wall or
the pelvic floor) that need to be made more loose.
Communication with the patient
during the examina-tion is important. An abrupt or stern command, such as
“Relax now; I’m not going to hurt you,” may raise the pa-tient’s fears, whereas
a statement such as, “Try to relax as much as you can, although I know that
it’s a lot easier for me to say than for you to do” sends two messages: (1)
that the patient needs to relax, and (2) that you recognize that it is
difficult, both of which demonstrate patience and un-derstanding. Saying
something such as, “Let me know if anything is uncomfortable, and I will stop
and then we will try to do it differently” tells the patient that there might
be discomfort, but that she has control and can stop the examination if
discomfort occurs. Likewise, stating, “I am going to touch you now” is helpful
in alleviating surprises. Using these statements demonstrates that the
examination is a cooperative effort, further empowering the patient in
facilitating care.
Related Topics