Chapter: Clinical Anesthesiology: Perioperative & Critical Care Medicine: Safety, Quality, & Performance Improvement
Quality of Care Performance Improvement Issues
QUALITY
OF CARE PERFORMANCE IMPROVEMENT ISSUES
It has long been recognized that quality and
safety are closely related to consistencyand reduction in practice variation.
The quality and safety movement(s) in medicine have their ori-gins in the work
of Walter Shewhart and his associ-ate W. Edwards Deming, who popularized the
use of statistics and control charts in evaluating the reli-ability of a
process. In manufacturing (where these ideas were initially applied), reducing
an error rate reduces the frequency of defective products and increases the
customer’s satisfaction with the prod-uct and the manufacturer. In medicine,
reducing the error rate (for everything from accurate timing and delivery of
prophylactic antibiotics to ensuring “cor-rect side and site” surgery and
regional anesthetic blocks) increases quality and reduces preventable injuries
to patients, while also eliminating the addi-tional costs resulting from those
errors.
Strategies to Reduce Performance Errors
Both in manufacturing and in medicine, there
is a natural tendency to assume that errorscan be prevented by better
education, better perfor-mance, or better management of individual workers. In other words, there is a tendency to look at
errors as individual failures made by individual workers, rather than as
failures of a system or a process. Using the latter point of view (as advocated
by Deming), to reduce errors one changes the system or process to reduce
unwanted variation so that random errors will be less likely. An outstanding
example of this is the universal protocol followed by health care insti-tutions
prior to invasive procedures. Adherence to this protocol ensures that the
correct procedure is performed on the correct part of the correct patient by
the correct physician, that the patient has given informed consent, that all
needed equipment and images are available, and that (if needed) the correct
prophylactic antibiotic was given at the correct time.
A related example of a simple approach to
improve safety and quality of a procedure is the use of a standardized
checklist, as described in the pop-ular press by Dr. Atul Gawande. The
importance of checklist use is addressed elsewhere in this text, for example in
the context of developing a culture of safety in the operating room. Such
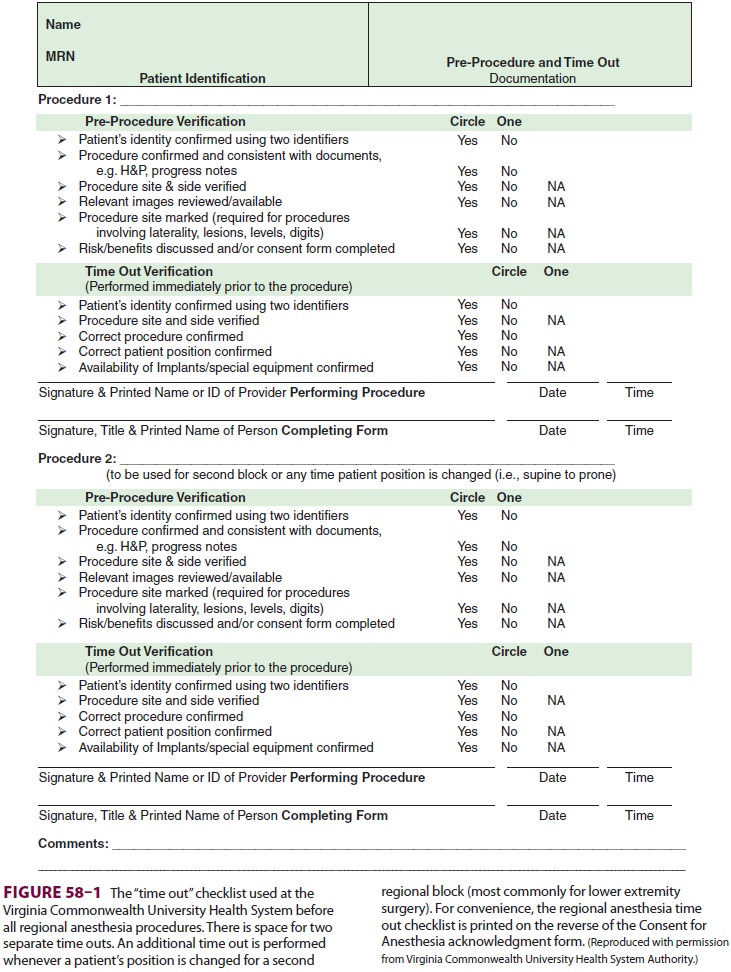
check-lists provide the “script” for the preprocedure uni-versal protocol (Figure
58–1). Studies have shown that the incidence of
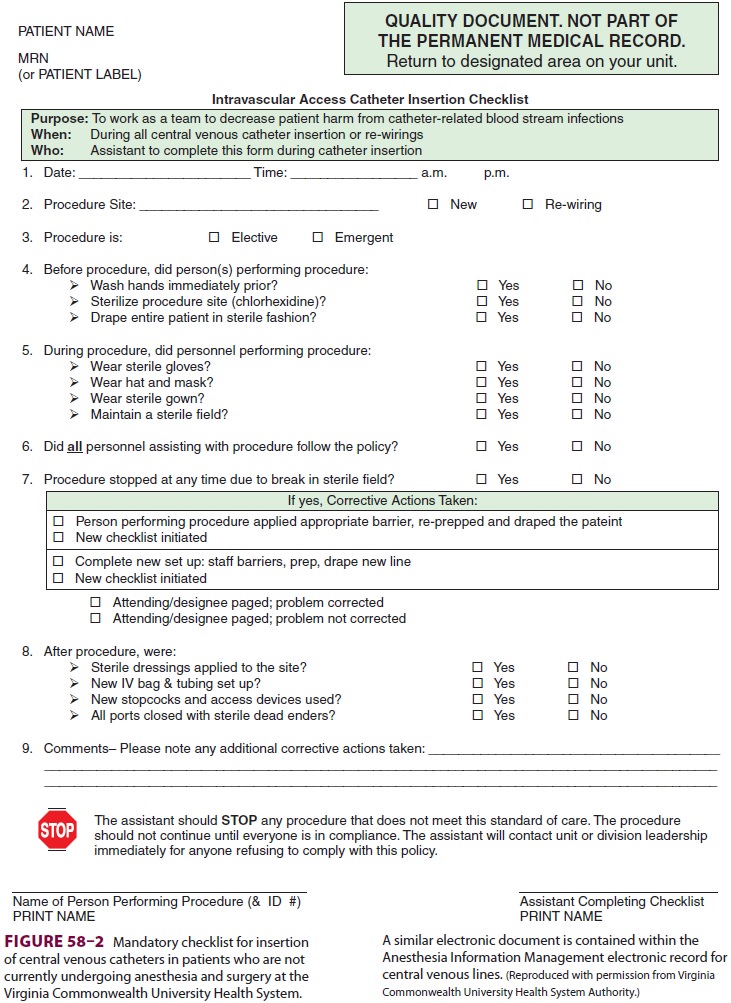
catheter-related bloodstream infections can be reduced when central venous
catheters are inserted after adequate cleansing and disinfection of the
operator’s hands by an operator wearing a surgical hat and mask, sterile gown,
and gloves; using chorhexidine (rather than povidone iodide) skin preparation
of the insertion site; and with sterile drapes of adequate size to maintain a
sterile field. Studies have also shown that use of all elements in this central
line “bundle” is much more likely when a checklist is required prior to every
central line insertion; a sample checklist is shown in Figure
58–2.
Benefits of Standardized Checklists
Checklists emphasize two important principles
about improving quality and safety in the surgical environment. First, using a
checklist requires that a physician communicate
with other members of the team. Good communication among team members improves
quality and prevents errors. It is easy to find examples of good communication
strategies. By clearly and forcefully announcing that protamine infusion has
been started (after extracorporeal perfusion has been discontinued during a
cardiac operation), the anesthesiologist helps prevent the surgeon and
perfusionist from making a critical error, such as resuming extracorporeal
perfusion without administering additional heparin. By accu-rately describing
the intended surgical procedure (at the time the patient is “posted” on the
surgical schedule), the surgeon helps prevent the operating room nurses from
making the critical error of not having the necessary instrumentation for the
pro-cedure, and helps prevent the anesthesiologist from performing the wrong
regional anesthetic proce-dure. We have selected these examples of good
com-munication because we are aware of adverse patient outcomes that resulted
from failure to transfer these specific points of information.
Second, using a checklist underscores the importance of ensuring that
every member of the surgical team has a stake in patient safety and good
surgical outcomes. The team member who records the checklist “results” is
usually not a physician but has the implicit authority to enforce adher-ence to
the checklist. On poorly functioning teams in which there is excessive
deference to authority figures, team members may feel that their opin-ions are
not wanted or valued, or may be afraid to bring up safety concerns for fear of
retaliation. On well-functioning teams, there is a “flattening” of the
hierarchy such that every team member has the authority and every team member
feels an obli-gation to halt the proceedings to prevent potential patient harm.
Quality Assurance Measures
In surgery there are well-recognized indicators of quality, such as having a very low incidence of surgical site infections and of perioperative mor-tality. However, at present there is no consensus as to the important measurements that can be used to assess quality of anesthesia care. Never-theless, surrogate anesthesia indicators have been monitored by a variety of well-meaning agencies. Examples include selection and timing of preop-erative antibiotics and temperature of patients in the postanesthesia care unit after colorectal sur-gery. Mindful of the importance of having accu-rate and relevant outcome measures, the ASA established the Anesthesia Quality Institute in 2009 and charged it with developing and collect-ing valid quality indicators for anesthetic care that can be used for quality improvement programs. Aggregation of the large amounts of data required for statistical validity is dependent on widespread adoption of electronic medical records (EMR) and anesthesia information management systems (AIMS). Currently these systems are present in a minority of hos-pitals in the United States. It is our hope that as their use becomes more widespread, the data and indicators that are collected and aggregated will provide greater insight into how quality of anes-thesia care may influence clinical outcomes that are important to patients.
Related Topics