Chapter: Essentials of Psychiatry: Childhood Disorders: Feeding and Other Disorders of Infancy or Early Childhood
Post Traumatic Feeding Disorder
Post Traumatic Feeding Disorder
Diagnostic Criteria
1. Food
refusal follows a traumatic event or repeated traumatic insults to the
oropharynx or gastrointestinal tract (e.g., chok-ing, severe vomiting, reflux,
insertion of nasogastric or en-dotracheal tubes, suctioning) that trigger
intense distress in the infant.
·
B. Consistent refusal to eat manifests in one of
the following ways:
·
Refuses to drink from the bottle, but may accept
food of-fered by spoon (although consistently refuses to drink from the bottle
when awake, may drink from the bottle when sleepy or asleep).
·
Refuses solid food, but may accept the bottle.
·
Refuses all oral feedings.
2.
Reminders of the traumatic event(s) cause distress
as mani-fested by one or more of the following:
·
Shows anticipatory distress when positioned for
feeding.
·
Shows intense resistance when approached with
bottle or food.
·
Shows intense resistance to swallow food placed in
the in-fant’s mouth.
3.
The food refusal poses an acute or long-term threat
to the child’s nutrition.
Epidemiology
Although no studies on the prevalence of this
disorder are avail-able, it appears that the occurrence of this feeding
disorder has been increasing because of the growing number of infants with
complex medical problems who survive.
Etiology
Although it is difficult to say what the inner
experience of a young infant might be, the affective and behavioral expressions
of in-fants provide a window to their inner life. In a study of infants
diagnosed with post traumatic feeding disorder, also including a control group
of healthy eaters and a group of anorectic infants matched by age, sex, race
and socioeconomic background, con-flict in mother–infant interactions during
feeding was present in both feeding-disordered groups. However, only those
subjects with a post traumatic feeding disorder demonstrated intense pre-oral
and intraoral feeding resistance. They appeared distressed, cried and pushed
the food away in anticipation of being fed, and kept solid food in their cheeks
or spat it out if the mothers were able to place any food in their mouths. The
mothers usually re-ported that these defensive behaviors started abruptly after
the infant experienced severe vomiting, gagging, or choking or un-derwent
invasive manipulation of the oropharynx (e.g., insertion of feeding and
endotracheal tubes or vigorous suctioning).
Diagnosis and Differential Diagnosis
This feeding disorder is characterized by the
infant’s consistent refusal either to drink from the bottle or to eat any solid
foods, and in most severe cases, by the infant’s refusal to eat at all.
De-pending on the mode of feeding that the infants appear to associ-ate with
the traumatic event(s), some refuse to eat solids, but will continue to drink
from the bottle, whereas others may refuse to drink from the bottle, but are
willing to eat solids. Some infants may put baby food in their mouths, but then
spit out any food that has any little lumps in it. Most infants get stuck in
these food patterns and may lose weight or lack certain nutrients because of
their limited diet.
Reminders of the traumatic event(s) (e.g., the
bottle, the bib, or the high chair) may cause intense distress for some
infants, whereby they become fearful when they are positioned for feed-ings
and/or presented with feeding utensils and food. They resist being fed by
crying, arching and refusing to open their mouths. If food is placed in their
mouths, they intensely resist swallowing. They may gag or vomit, let the food
drop out, actively spit the food out, or store the food in their cheeks and spit
it out later. The fear of eating seems to override any awareness of hunger.
There-fore, infants who refuse all foods, including liquids and solids, require
acute intervention due to dehydration and starvation.
In addition to a thorough history about the onset
of the infant’s food refusal and the medical and developmental history, the
observation of the infant and mother during feeding is critical for
understanding this feeding disorder and differentiating it from infantile
anorexia and from sensory food aversions. It is helpful to ask the mother to
bring a variety of foods, including those that the infant refuses and those
that he or she accepts. Infants with a post traumatic feeding disorder
characteristically appear en-gaged and comfortable with their mothers as long
as the feared food is out of sight. Some infants begin to show distress when
they are placed in the high chair and they struggle to get away. In less severe
cases, the infant might allow the food to go into the mouth but then spit it out
and show distress only when urged to swallow. This anticipatory fear of food
differentiates infants with a post traumatic feeding disorder from anorectic
infants, whose food refusal appears random and related to issues of control in
the relationship with the mothers. Toddlers with sensory aversions to certain
types of food might also show distress when urged to eat these foods. However,
their mothers do not remember a traumatic event that seemed to trigger the food
refusal behaviors.
Course and Natural History
Most infants seem to get locked into their food
refusal patterns. The more anxiously the parents react to the infant’s food
refusal, the more anxious the infants appear to become, with the parent and the
infant feeding off each other’s anxiety. Individual case studies indicate that
some of these infants depend for years on gastrostomy feedings to survive.
Others may live on milk and puréed food until school age, when the social
embarrassment of their eating behavior urges the parents to seek help.
Treatment
Because of the complexity of many of these cases, a
multidisci-plinary team (consisting of a pediatrician or gastroenterologist, a
psychiatrist or psychologist, a social worker, an occupational therapist or
hearing and speech specialist, a nutritionist and a specially trained nurse to
serve as team coordinators) is best equipped to meet all the needs of these
infants and their parents.
Before any psychiatric treatment can be
successfully initi-ated, the medical and nutritional needs of the infant need
to be addressed. In severe cases of total food refusal, it is important to act
quickly to maintain the infant’s hydration. The medical and psychiatric team
members must work together to assess whether temporary nasogastric tube
feedings are indicated or whether plans for a gastrostomy should be made.
Unfortunately, the re-peated insertion of nasogastric feeding tubes can
intensify a post traumatic feeding disorder, and an infant in a labile medical
con-dition can take months if not years to recover.
The psychiatric treatment of this feeding disorder
involves a desensitization of the infant to overcome the anticipatory anxi-ety
about eating and return to internal regulation of eating in re-sponse to hunger
and satiety. It is most important to help the par-ents understand the dynamics
of a post traumatic feeding disorder so that they can recognize the infant’s
anticipatory anxiety and become active participants in the treatment. After
identification of triggers of anticipatory anxiety (e.g., the sight of the high
chair, the bottle, or certain types of food), a desensitization by gradual
exposure can be initiated or a more rapid desensitization through more
intensive behavioral techniques can be implemented.
With both techniques, it is important to have a
professional assess the infant’s oral motor coordination because many infants
who refuse to eat for extended periods fall behind in their oral motor
development due to lack of practice. The rapid introduc-tion of table food to a
child who has delayed oral motor skills may lead to choking, thereby creating a
setback to the desensitization process.
During the desensitization process, the infant has
to be re-inforced for swallowing the food. This behavioral manipulation of the
infant’s eating frequently leads to external regulation of eating in response
to the reinforcers. Once the infant has become comfortable with eating, it is
important to phase out these exter-nal reinforcers to allow the infant to
regain internal regulation of eating in response to hunger and fullness. This
can be a difficult transition because many infants gain control over their
parent’s emotions by eating or not eating. The techniques described under
infantile anorexia – the implementation of the feeding guidelines contained in
step 3 – can be helpful in making this transition.
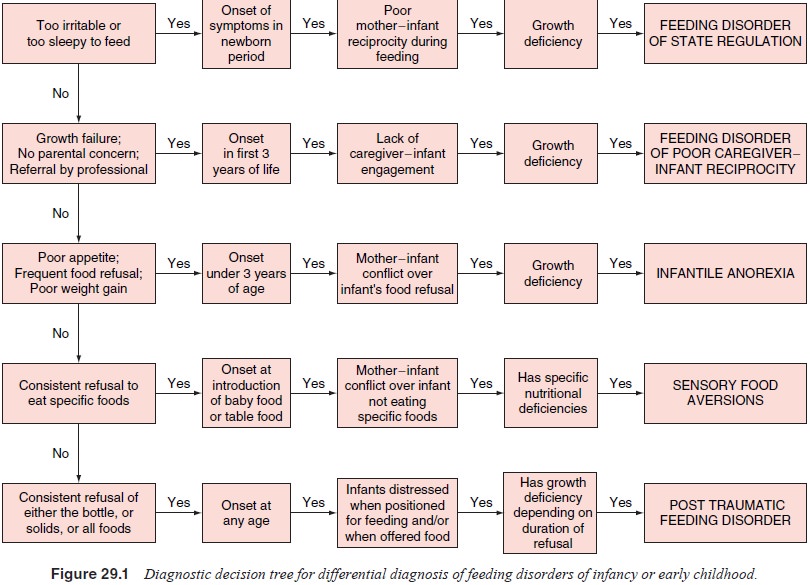
As summarized in Figure 29.1, each of these five
feeding disorders presents with specific symptom patterns and charac-teristic
mother–infant interactions, which help to diagnose and differentiate the
various feeding disorders. The correct diagno-sis is critical because a
treatment that is helpful for one feed-ing disorder may be ineffective or even
worsen another feeding disorder. For example, infants with infantile anorexia
become more aware of their hunger cues and feed better if fed only every4 hours
without being offered food or liquids in between meals. However, an infant with
post traumatic feeding disorder who is afraid of eating will not accept food
regardless of how long he or she has been kept without feeding. On the other
hand, behav-ioral techniques that help extinguish fear-based food refusal in a
post traumatic feeding disorder further distract an infant with infantile
anorexia and further interfere with the awareness of hunger.
Related Topics