Chapter: Essentials of Psychiatry: Physician–Patient Relationship
Physician–Patient Relationship
Physician–Patient Relationship
For centuries, healers had little understanding of
disease and lacked the technologies we now know are necessary for the treatment
and cure of many diseases. Physicians had few medications, and surgery was only
a last resort. In fact, the most important tool for healing was the
relationship between the physician and the patient. Interpersonal relationships
have a powerful influence on both morbidity and mortality (House et al., 1988). Social connectedness
enhances health in both direct and indirect ways: directly regulating many
biological functions, decreasing anxiety, providing opportunities for new
information, and fostering alternative behaviors (Hofer, 1984). We know little
about the basic mechanisms by which interpersonal relationships, and the
physician–patient relationship in particular, operate (Ursano and Fullerton
1991). However, clinical wisdom holds that both the reality-based elements of
the physician–patient relationship – in modern times referred to as the working
alliance or the therapeutic alliance (Zetzel, 1956; Greenson, 1965) – and the
fantasy-based elements of that relationship affect the patient’s pain,
suffering and recovery from illness.
Physicians learned through trial and error to
interact with their patients in ways that relieved pain and promoted health
(Frank, 1971). Often the physician’s only interventions were reassuring
patients, providing knowledge about the patient’s disease, accept-ing the
patient’s feelings of distress as normal, and maximizing the patient’s hope for
the future. Although these interventions, based on wisdom and intuition, are no
longer the only tools available to the physician, they continue to be an
important part of the physician’s and particularly the psychiatrist’s
therapeutic armamentarium.
Such nonspecific aspects of cure are often thought
to be mystical or mysterious. In fact, in biological studies they are
rec-ognized as the placebo effect. Oddly, these effects of interper-sonal
relationships are both one of the prized and one of the most denigrated aspects
of all of medicine. Yet, as clinicians, we all strive to alleviate our
patients’ pain and suffering and return them to health as soon as possible with
whatever tools may help. Many well-designed studies show that 20 to 30% of
subjects respond to the placebo condition. Recent studies show that analgesic
pla-cebo has similar neural mechanisms to opioid analgesia (Petrovic et al., 2002). The problem with placebos
is not whether they work but that we
do not understand how they work and, therefore, we do not have control over
their effects. As a physician, one strives to maximize one’s interpersonal
healing effects and, in this way as well as with other healing tools, increase
the chances of our patients’ relief from pain and of recovery.
The physician–patient relationship includes
specific roles and motivations. These form the core ingredients of the
healingprocess. In its most generic form the physician–patient relation-ship is
defined by the coming together of an expert and a help seeker to identify,
understand and solve the problems of the help seeker. The help seeker (in
modern terms, the patient) is moti-vated by the desire and hope for assistance
and relief from pain (Sullivan, 1954). A physician is required to have a
genuine interest in people and a desire to help (Lidz, 1983). Simply stated,
“the se-cret of the care of the patient is in caring for the patient” (Peabody,
1927). Caring about and paying attention to a patient’s suffering can yield
remarkable therapeutic dividends. More than one attend-ing physician has been
reminded of this when a patient deferred making a treatment decision until he
or she was able to consult with “my doctor”, who turned out to be the medical
student.
In today’s technology-driven medicine, the
importance and complexity of the physician–patient interaction are often
over-looked. The amount of information the medical student or resident must
learn frequently takes precedence over learning the fine points of helping the
patient relax sufficiently to provide a thorough his-tory or to allow the
physician to palpate a painful abdomen. Talk-ing with patients and
understanding the intricacies of the physi-cian–patient relationship may be
given little formal attention in the medical school curriculum. Even so, medical
students, residents and staff physicians recognize, often with awe, the skill
of the sen-ior physician who uncovers the lost piece of history, motivates the
patient who had given up hope, or is able to talk to the distressed family
without increasing their sense of hopelessness or fear.
The relationship between the physician and the
patient is es-sential to the healing of many patients, perhaps particularly so
for many psychiatric patients. The physician who can skillfully recog-nize the
patient’s half-hidden comment that he or she has not been taking the prescribed
medication, perhaps hidden because of feel-ings of shame, anger, or denial, is
better able to ensure long-term compliance with medication as well as to
motivate the patient to stay in treatment. Regardless of the type of treatment
– medication, biofeedback, hospitalization, psychotherapy, or the rearrangement
of the demands and responsibilities in the patient’s life – the rela-tionship
with the physician is critical to therapeutic outcome.
Modern medicine emphasizes a specific role for the
physi-cian in the relationship with the patient. In many Western coun-tries,
the patient comes for help with a specific problem, the doctor’s office staff
secures permission from a third party payer for the doctor to conduct a
particular treatment, a prescribed intervention, which will take a specified
amount of time. Dec-ades ago, when the doctor was neighbor, advisor and friend
to the patient and routinely invited to important family events inthe patient’s
life such as weddings of children, and when doctors routinely cared for more
than one generation of the same family, the physician typically assumed that he
or she would be a source of strength and assistance to the patient throughout
the cycle of life. This meant more than curing a specific disease or relieving
a specific pain.
While today’s patients may not consciously expect
that the physician’s influence and healing powers will take many forms in a
complex interpersonal relationship, human nature is still the same, and
patients still want from their doctors many nonspe-cific forms of emotional
support which can promote a sense of well-being and better health. Though
modern doctors may feel a great deal of time pressure to see many patients each
day and to focus narrowly their healing efforts, the physician must also be
sensitive to the many needs of patients, who believe that the physician is
possessed of wisdom and understanding. Sensitivity to such desires and needs
will promote effective medical care in all specialties, with all patients. A
view that such patients are unusually needy and demanding will not serve the
cause of ef-fective medical care.
Finally, in today’s mobile and geographically
evermore united world, the importance of recognizing the needs of patients from
parts of the world other than that of the physician’s is a chal-lenge to the
practitioner. The physician must be open to the limita-tions of his or her
knowledge of the expectations, beliefs and likely behavior of patients from
different cultures, nations, religions, and ethnic and socioeconomic
backgrounds. The physician must rec-ognize this challenge and one hopes,
embrace it with enthusiasm. It can make the practice of medicine a more
exciting experience.
The physician–patient relationship is also a source
of information for the physician. The way the patient relates to the physician
can help the physician understand the problems the patient is experiencing in
her or his interpersonal relation-ships. The nature of the physician–patient
relationship can also provide information about relationships in the patient’s
child-hood family, in which interpersonal patterns are first learned. With this
information, the physician can better understand the patient’s experience,
promote cooperation between the patient and those who care for her or him, and
teach the patient new behavioral strategies in an empathic manner,
understanding the patient’s subjective perspective, that is, feelings, thoughts
and behaviors.
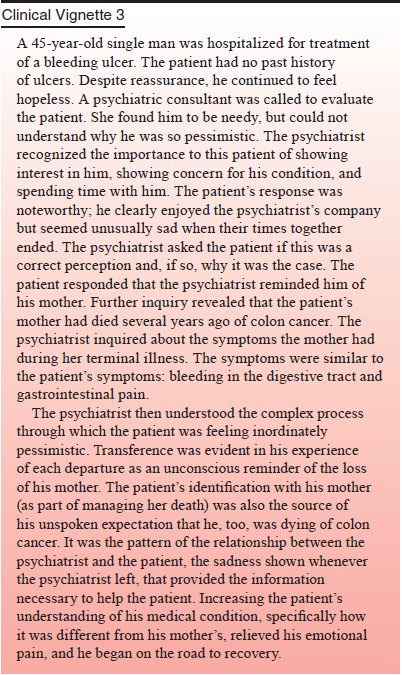
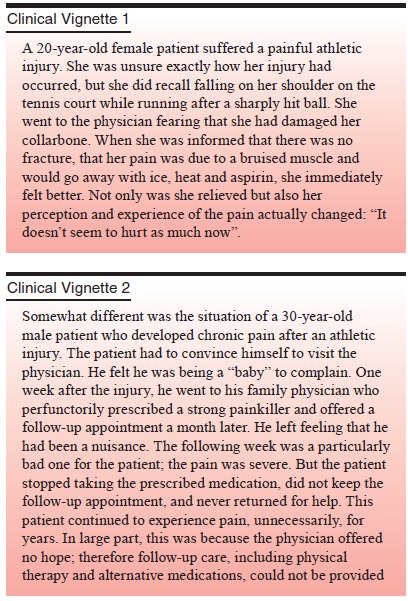
These clinical vignettes illustrate that the
physician–patient relationship is composed of both the reality-based component
(the working alliance or therapeutic alliance) and the fantasy-based component
(the transference) derived from the patient’s patterns of interpersonal
behavior learned in childhood. Either or both of these may maximize or limit
the patient’s sense of reassurance, available information, feelings of comfort
and sense of hope (Meissner, 1996). In this way, the nonspecific curative as-pects
of the physician–patient relationship may be enhanced or diminished.
Related Topics