Chapter: Essentials of Psychiatry: Substance Abuse: Nicotine Dependence
Phases of Treatment - Nicotine Dependence
Phases of Treatment
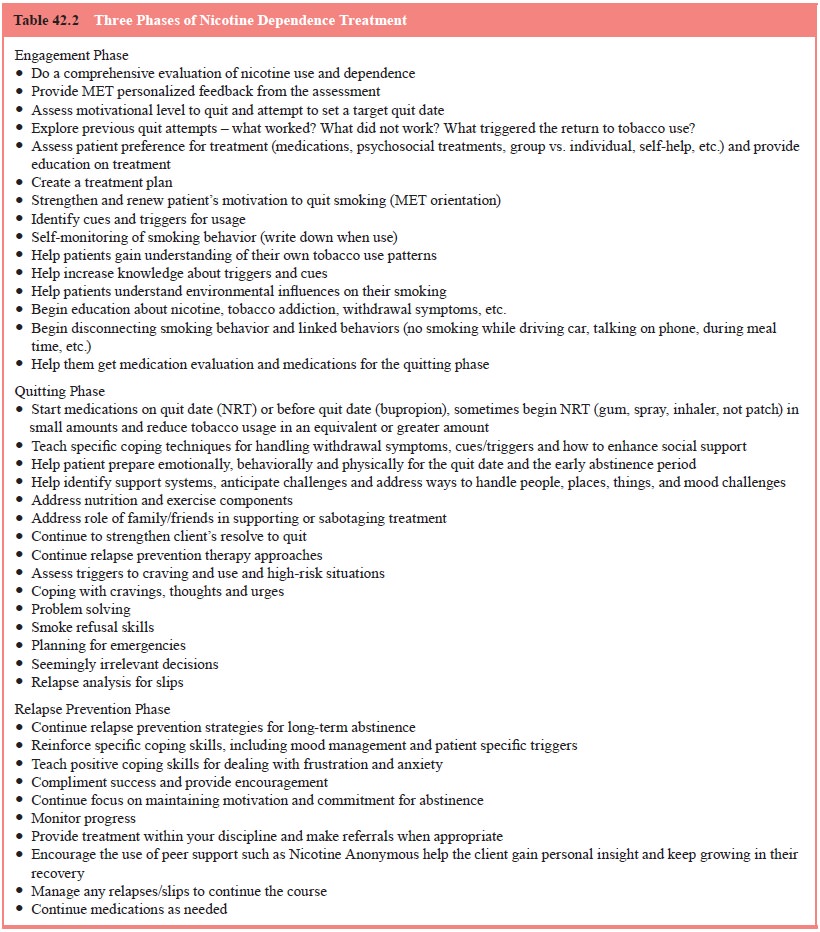
The general approach to the treatment of nicotine
dependence considers three phases of treatment (engagement, quitting, and
relapse prevention) (Table 42.2).
The importance of each of the biopsychosocial
factors in initiating and maintaining smoking can vary considerably in
dif-ferent individuals. As a result, smoking cessation interventions should be
tailored to the individual and his or her particular circumstances. This may be
one reason why “one size fits all” generic treatment interventions have had
such a low success rate. It must also be kept in mind that nicotine dependence
is as complex in its components and determinants as other addictions and that
more comprehensive multicomponent treatments may be required. When a smoker is
ready for a cessation attempt, a “quit date” should be selected. After
cessation, close monitoring should occur during the early period of abstinence.
Before the quit date, the person should be encouraged to explore and organ-ize
social support for the self-attempt. Plans to minimize cues associated with
smoking (e.g., avoiding circumstances likely to contribute to relapse) are
important, as is considering alterna-tive coping behaviors for situations with
a higher potential for relapse. A telephone or face-to-face follow-up during
the first few days after cessation is critical because this is the time that
with-drawal symptoms are most severe, with 65% of patients relapsing by 1 week.
A follow-up face-to-face meeting within 1 to 2 weeks allows a discussion of
problems that have occurred (e.g., difficul-ties managing craving) and serves
as an opportunity to provide reinforcement for ongoing abstinence. Even after
the early period of abstinence, periodic telephone or face-to-face contacts can
provide continued encouragement to maintain abstinence, allow problems with
maintaining abstinence to be addressed, and pro-vide feedback regarding the
health benefits of abstinence.
If an initial attempt at cessation using only
information and brief advice from the physician has been unsuccessful,
phar-macotherapy may be used unless contraindications are present or unless the
person has had few or no significant withdrawal symptoms. The most common
pharmacotherapy approaches are nicotine replacement therapies (NRTs: patch,
gum, spray, or in-haler) or bupropion for nicotine dependence. Combining
differ-ent types of NRT and bupropion is becoming more common in clinical
practice, including using these medications for at least several months and in
some cases 1 year or longer. Maintenance medications are being considered in an
effort of harm reduction in a more select group of patients. If a
detoxification/quit attempt with pharmacotherapy alone fails, psychosocial
treatments and the use of higher NRT dosages/multiple medications are possi-ble
clinical next steps. Psychosocial treatments are often avail-able through
organizations such as the American Cancer Society, American Lung Association,
the American Heart Association, or through local hospitals that provide health
prevention and public education programs (American Cancer Society/National
Cancer Institute, 1989). If pharmacotherapy is unacceptable or
con-traindicated, behavioral therapy (BT) alone should be provided. Failure with
pharmacotherapy or BT alone suggests the need for more detailed in-depth
assessment and more intensive and mul-timodal interventions.
Related Topics