Chapter: Modern Pharmacology with Clinical Applications: Muscarinic Blocking Drugs
Muscarinic Blocking Drugs: Pharmacological Actions
PHARMACOLOGICAL
ACTIONS
Muscarinic antagonists have no intrinsic activity, and they can
produce effects only by blocking the activation of muscarinic receptors by
muscarinic agonists or by neuronally released ACh. Therefore, the magnitude of the response produced by muscarinic
antagonists de-pends on the existing level of cholinergic activity or on the
presence of muscarinic agonists. Also, the nature of the response of an organ
to the administration of a muscarinic antagonist will depend on the organ’s
pat-tern of innervation; for example, some organs receive dual innervation from
adrenergic and cholinergic path-ways. At these locations, block of the
activation of mus-carinic receptors can increase the tone provided by the adrenergic
input.
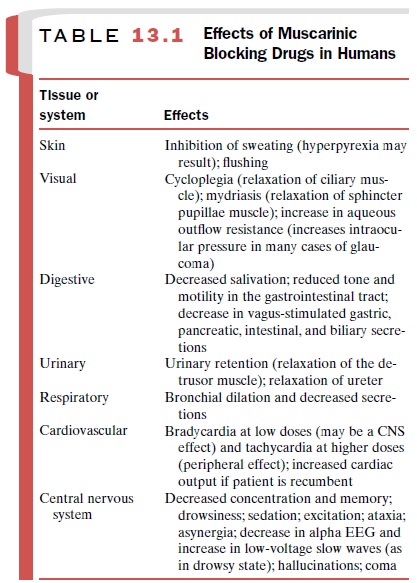
The effects of muscarinic
blocking drugs on various human organ systems are summarized in Table 13.1. The
tissues or systems affected will depend on the dose ad-ministered, the drug’s
pharmacokinetic properties (e.g., increased entry into the CNS at higher
concentrations), and the differential sensitivity of muscarinic receptors in
various organs to individual blocking agents. Although muscarinic agonists typically do not exhibit
selectivity among muscarinic receptors , some muscarinic antagonists are selective in their ability to block subtypes of
muscarinic receptors.
Heart
Intravenous administration of
low doses of atropine or scopolamine often produces slight bradycardia, whereas
higher doses produce tachycardia by directly blocking the parasympathetic input
to the sinoatrial node. Although it has been suggested that the bradycardia
re-sults from an effect of the drugs on the CNS (thought to be central vagal
stimulation), this appears unlikely, since methylatropine (a quaternary
ammonium deriva-tive of atropine) produces a similar response. One plau-sible
explanation for the paradoxical
bradycardia pro-duced by low doses of muscarinic blockers is that they
block presynaptic muscarinic receptors that normally provide feedback
inhibition of the release of ACh. Antagonism of these presynaptic muscarinic
receptors prevents feedback inhibition and increases the release of ACh, and
this effect may dominate postsynaptic mus-carinic receptor blockade produced by
low doses of an-tagonist. Atropine can also facilitate atrioventricular (A-V)
conduction and block parasympathetic effects on the cardiac conduction system
and on myocardial con-tractility.
Blood Vessels
Atropine and other muscarinic
antagonists produce minimal effects on the circulation in the absence of
cir-culating muscarinic agonists. This reflects the relatively minor role of
cholinergic innervation in determining vascular smooth muscle tone. Atropine
can produce flushing in the blush area owing to vasodilation. It is not known
whether this is a direct effect or a response to the hyperthermia induced by
the drug’s ability to inhibit sweating.
Gastrointestinal Tract
Muscarinic antagonists have
numerous effects on the digestive system . The inhibition of salivation by low
doses of atropine results in a dry mouth and difficulty in swallowing.
Antimuscarinic drugs also inhibit gastric acid secretion and gastroin-testinal
motility, because both processes are partly un-der the control of the vagus
nerve. Relatively large doses of atropine are required to inhibit acid
secretion, and side effects such as dry mouth, tachycardia, ocular
disturbances, and urinary retention are drawbacks to the use of muscarinic
antagonists in the treatment of peptic ulcers.
Bladder
Muscarinic antagonists can
cause urinary retention by blocking the excitatory effect of ACh on the
detrusor muscle of the bladder. During urination, cholinergic in-put to this
smooth muscle is activated by a stretch reflex.
Central Nervous System
Although atropine and
scopolamine share many prop-erties, an important difference is the easier entry
of scopolamine into the CNS. Typical doses of atropine (0.2–2 mg) have minimal
central effects, while larger doses can produce a constellation of responses
collec-tively termed the central
anticholinergic syndrome. At intermediate doses (2–10 mg), memory and
concentra-tion may be impaired, and the patient may be drowsy. If doses of 10
mg or more are used, the patient may ex-hibit confusion, excitement,
hallucinations, ataxia, asyn-ergia, and possibly coma.
Even low doses of scopolamine
have central effects. Sedation, amnesia, and drowsiness are common during the
clinical use of this drug. Large doses of scopolamine can produce all of the
responses seen with atropine. Other tertiary amine compounds with muscarinic
re-ceptor blocking activity have similar central effects.
Eye
Antimuscarinic drugs block
contraction of the iris sphincter and ciliary muscles of the eye produced by
ACh. This results in dilation of the pupil (mydriasis)
and paralysis of accommodation (cycloplegia),
responses that cause photophobia and inability to focus on nearby objects.
Ocular effects are produced only after higher parenteral doses. Atropine and
scopolamine produce responses lasting several days when applied directly to the
eyes.
Lung
Muscarinic antagonists
inhibit secretions and relax smooth muscle in the respiratory system. The
parasym-pathetic innervation of respiratory smooth muscle is most abundant in
large airways, where it exerts a domi-nant constrictor action. In agreement
with this innerva-tion pattern, muscarinic antagonists produce their greatest
bronchodilator effect at large-caliber airways.
By this mechanism they can
block reflex laryngospasm during surgery. In addition, these drugs are potent
in-hibitors of secretions throughout the respiratory sys-tem, from the nose to
the bronchioles.
Nicotinic Receptors
Although the antimuscarinic
drugs are normally selec-tive for muscarinic cholinergic receptors, high
concen-trations of agents with a quaternary ammonium group (e.g.,
propantheline) can block nicotinic receptors on autonomic ganglia and skeletal
muscles. However, these effects are generally not clinically important at usual
therapeutic doses.
Related Topics