Chapter: Maternal and Child Health Nursing : Obstetric Conditions that Complicate Pregnancy
Multiple Pregnancy
Multiple Pregnancy
When
there is more than one fetus in- utero
the term 'plural' or 'multiple' pregnancy is applied. Twins occur approximately
once in about every 90 pregnancies, and the tendency is manifest in certain
families.
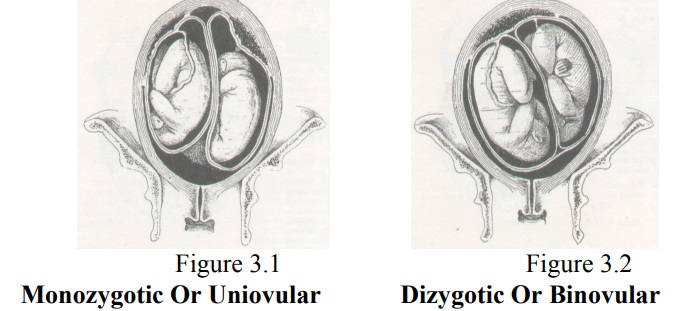
Monozvgotic (Uniovular)
Monozygotic
or single ovum twins are known ^as identical twins because their physical and
mental characteristics are so similar. They develop from one ovum which has
been fertilised by one spermatozoon and are always of the same sex. They are
definitely uniovular if they share one placenta and one chorion; a few have two
chorions. There is a connection between the circulations of blood in the two
babies. Finger and palm prints are identical in monozygotic twins.
Errors in
development are more likely in monozygotic twins, so abnormal fetuses are more
common: conjoined twins, usually known as Siamese, are uniovular in type- The perinatal
mortality rate is higher than in dizygotic twins.
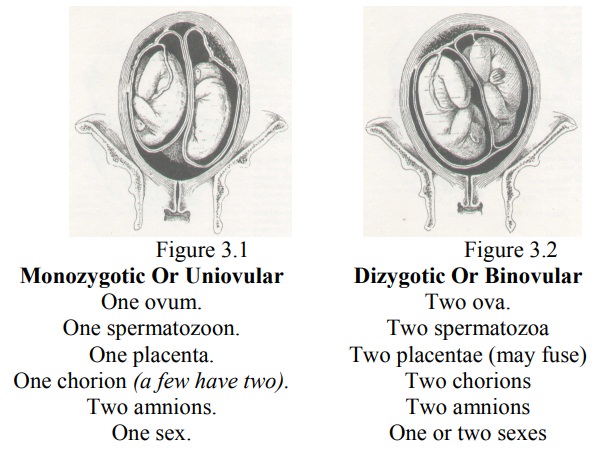
Dizygotic (Binovular)
Dizygotic
or double ovum twins, which are three
times more common than uniovular twins, develop from the fertilisation of two
ova and two spermatozoa. The babies may or may not be of the same sex and their
physical and mental characteristics can be as different as in any two members
of one family. Dizygotic twin bearing is hereditary mainly via the mother. They each have a separate placenta and chorion,
but, although the placentae may
fuse.
Fetal circulations do not mix. The differentiation between monozygotic and
dizygotic twins at birth is not always easy, because some monozygotic twins
have two chorions.
If the
babies are of different sexes or have two separate placentae, they are
definitely dizygotic. But sometimes the two zygotes embed close to each other
so that the placentae fuse and appear to the naked eye to be one single
placenta. In that case.if the sex of the babies is the same, diagnosis is made
by examination of the membranes of the fetal sac, in dizygotic twins two
chorions are present.
Very
occasionally one fetus may die and be retained in utero until term when it will be expelled with the placenta as a
flattened paper-like fetus—a fetus papyraceous. Although twin babies are as a
rule small and often preterm, ranging from 2260g to 2720g, normal weights are
not uncommon; the author having seen twins weighing 4060g and 3960g; 4340g and
4300g.
Diagnosis of twins
The
diagnosis of twins is not always easy in primigravidae with firm abdominal
walls, or in obese women, and experienced doctors and midwives may not always
detect them. The period of gestation is also difficult to assess.
An ultrasonic
scan will demonstrate two heads at 15 weeks; two gestational sacs have been
seen at eight weeks. X-rays may be used after the 30th week.
Twins may
first be diagnosed by finding the uterus large and the fundus well above the
umbilicus after the birth of the first baby.
On inspection
Suspicious
is aroused when the uterus is unduly large for the period of gestation after
the 20th week. The uterus looks round or broad and fetal movement
may be seen over a wide area, but this is not diagnostic. At term, a woman of
average build has an abdominal girth of about 100cm. the possibility of
polydramnios must be considered, and it can be present in conjunction with or
independent of twins, but palpation should help to conclude the diagnosis.
On palpation
Finding
two heads is diagnostic. If one fetus lies in front of the other, it may not be
easy to detect two heads or two backs. Should the fetal head seem small in
comparison with the size of the uterus this rather suggests the presence of two
fetuses. Excessive fetal parts might make one suggest that twins were present.
Auscultation
Hearing
two fetal hearts is not a reliable method of diagnosis because with a large,
vigorous fetus, the fetal heart can sometimes be heard over a wide area.
The Effect of Twins on Pregnancy
Pre-eclampsia is more common than in single
pregnancies.Polyhydramnios. Acute
polyhydramnios is invariably associatedwith uniovular twins ,the usual outcome
being abortion.
Anaemia develops because of the increased
fetal demands foriron:
The minor disorders and
general discomforts of pregnancy aremore pronounced: morning sickness, nausea
and heartburn are more persistent.
Pressure symptoms due to the
weight and size of the uterus maybe troublesome,
·
The tendency to oedema of the ankles and varicose
veins is increased because of pressure on the veins returning blood from the
lower limbs,
·
Dyspnoea and indigestion are more marked: backache
is common.
Management of Pregnancy
As soon
as twins are diagnosed a close check should be kept on the mother's haemoglobin
and advice given regarding foods rich in iron.
Ferrous
preparations are usually prescribed and vitamin supplements are essential.. The
woman should drink at least 1200 ml of milk daily to prevent her calcium
reserves from being depleted.
Her
protein intake must be adequate.
In order
to detect pre-eclampsia which is three times more common in multiple pregnancy,
the woman is seen weekly from the time twins are diagnosed about the 20th week.
To
relieve the discomfort of a heavy uterus, a good supporting maternity belt will
be appreciated.
Extra
pillows are needed for sleep, as the woman feels more comfortable when propped
up. Adequate rest is essential during the last 12 weeks to increase uterine
blood flow.
The woman
may be admitted to hospital from the 30th to the 36th week to avoid preterm
labour by providing rest, and to improve her nutrition. She should not be
permitted to go beyond term but many go into labour prior to then.
The Effect of Twins on Labour
Although,
multiple pregnancy may not be regarded as abnormal in itself, many
complications that endanger fetal and maternal life do arise . Labour is often
preterm: the babies tend to be light for date even when at term.
The
perinatal mortality rate is higher than in single births. The mortality rate of
the second twin is twice that of the first, and this may be due to reduction in
the placental circulation and partial separation of placenta following the
birth of the first twin.
Malpresentation
is more common. For these reasons hospitalization for delivery is advocated.
The Management of Labour
Heavy
sedation should be avoided.
Epidural
analgesia may be use.
If delay
occurs due to hypotonic uterine action after the delivery of the first twin an
oxytocin drip may be given after puncture of the membranes and kept running
until one hour after both babies and placenta are delivered.
Preparations
should be made for the reception of two immature babies, who may show signs of
asphyxia or intracranial injury.
Woman
should be observed for signs of shock due to sudden reduction in abdominal
pressure.
Active Treatment
The woman
may be more comfortable in the dorsal position with additional pillows.
Perineal
infiltration or pudendal nerve block is commonly employed and an episiotomy is
made in an endeavour to lower thehigh
perinatal mortality rate.
The
airway of the first baby is cleared. The cord should be ligatured in two
places, for although the placental end of the cord is tied or clamped at every
delivery, it is because of the possibility of undiagnosed monozygotic twins
that this is done. The first baby, after being marked No. 1, is laid in a warm
cot and the midwife keeps her 'ear and
eye on it.
The
abdomen is palpated without delay to ensure that the lie of the second twin is
longitudinal. Presentation and position are diagnosed, but are of less
importance: the fetal heart is listened to. The midwife stands by. She will
closely observe the uterus, probably keeping her hand lightly on it to detect
uterine contractions. The fetal heart should be checked frequently.
With
three or four good contractions and the woman pushing effectively the second
baby ought to be born. But if, when 5 minutes have elapsed, contractions have
not recommenced, the midwife should scrub up and after making sure that the
head or the breech is presenting she should puncture the bag of membranes and
massage the uterus to stimulate uterine action. The second baby should be born
within 15 minutes after the first baby.
Ergometrine,
0.5mg or Syntometrine, 1ml, should be given intramuscularly as soon as both
placentae are born to prevent postpartum haemorrhage. If Syntometrine is given
inadvertently after the birth of the first baby, the second baby must be
expelled immediately by fundal pressure. Midwives must always remember the
possibility of an undiagnosed twin when they administer Syntometrine during the
actual birth of a baby. The woman should not be left until at least two hours
after the birth of the palcentae and to ensure sleep a sedative is given.
Avoid
unnecessary delay in the delivery of the second as this may result in:
The fetus
in utero may die of anoxia should the palcenta separates.
The risk
of sepsis is increased when the cord is lying outside the vulva.
The
cervix closes to a certain extent and will have to dilate again. Having ensured
that the lie is longitudinal, the doctor will probably puncture the membranes,
and give an oxytocin drip, when the uterus begins to contract he may apply
forceps or use the Malmstrom vacuum extractor.
The expulsion of a placenta or bleeding before
the birth ofthe second twin gives warning that the placenta still in- utero may
also be separating and causing hypoxia of the unborn twin; in which case, the
midwife should massage the uterus and expel the second twin as soon as possible
by using fundal pressure. (The usual sequence of events is for both babies to
be born and then the placentae).
Locked twins are very rare indeed, and the
most seriousvariety occurs when the first fetus is presenting by the breech and
the head of the second fetus which is presenting by the vertex gets in front of
the after coming head of the first baby. The heads become impacted and
decapitation of the head of the first baby is usually necessary.
Management of the Puerperium
Involution
of the uterus may be slow; after pains are more troublesome. The care of the
babies is a most urgent problem, as the number of twin babies who die is
alarmingly high, the smaller one may be light for date. The mother will need
help and advice in regard to feeding, and should not be discharge from hospital
until the babies are gaining weight satisfactorily.
Conclusions
Some conditions that affect the health of the woman during pregnancy are directly related to the pregnancy itself. They add more risk to the mother and the fetus while some lead to greater emotional and financial difficulties e.g. multiple pregnancy. Early diagnosis of these conditions prevents the serious effect on the pregnancy, labour and puerperium. Women with previous history of these conditions must register early and pay more visits to the clinic for close monitoring of their condition.
Related Topics