Chapter: Maternal and Child Health Nursing : Labour
Labour
Labour
Introduction
In the
previous units of this module, we have learnt much about pregnancy and care
during the prenatal period. In this unit we will learn about the remarkable events
that result in delivery of the baby. We shall discuss the physiology of labour,
the factors that causes the onset of labour, signs of labour and how to
alleviate the woman’s sufferings in labour.
Objectives
At the
end of lesson the learner will be able to
·
Describe the changes that occur in the uterine
tissue during labour.
·
Describe the stages of labour
·
Explain the spontaneous process of labor and how
this may be enhanced or inhibited.
·
Plan and time care in order to optimize the
well-being of both the mother and the baby during the course of labour.
Definitions
Labour is
descried as the process by which the fetus, placenta and membranes are expelled
through the birth canal after 24 weeks of gestation .
Normal labour
Is the
process by which the fetus is born at term (after 37 wks gestation vertex
presenting, spontaneous in onset (natural unaided effort of the mother) with 18
hours and without injury to the mother and the baby.
Labour
does not involve only the physical stamina but it involves emotional control.
The event that happened during labor can affect the relationship between mother
and child and influence subsequent pregnancies. Labour is influenced by three
factors.: the powers that is ,the contractions, the passages that is, the birth
canal and finally the passenger which is the fetus
Stages of labour
Labour is
described in three stages the fourth stages is the first one hour after the
delivery of placenta.
1. The First Stage
“ This is the period from the onset
of the true regular uterinecontractions until full dilatations of the cervical
Os.” This is the period of cervical dilatation and it is described in phases.
Latent Phase: this is the period prior to
active stage oflabour. Time from spontaneous onset of labour until the cervix
is 3-4cm dilated and the cervix shortens from 3cm to 0.5cm long. It may last
6-8hours in primip but much shorter in multiparous, the line on the partogram
remains horizontal.
Active phase: Is the period from 3-4cm to 10cm
dilatation.The cervix undergoes more rapid dilatation, at the rate of about 1cm
per hour. The line on the partogram rises rapidly. It last 2-6 hours but
shorter in multiparous women.
2. Second Stage
This is
that of expulsion of the fetus. “it is the period from full dilatation of the
cervix and the urgue to push and ends when the fetus is expelled”.
3. The Third Stage
Is that
of separation and expulsion of placenta and membranes and the control of
bleeding. “That is from the birt h of the baby until the delivery of the
placenta and membranes and bleeding is controlled”. Not affected by parity.
4. The fourth stage:
This is a
period of one hour following the birth of placenta. This period is given
recognition in order to emphasis the importance of continuous vigilance on the
woman for the risk of post partum hemorrhage. Not affected by party. It is
actually the first one hour in puerperium.
Duration of labor
There are
wide variations in the duration of labor. The length of labor is influenced by
party, time of the last delivery, type of pelvis, size and presentation of the
fetus, strength and frequency of uterine contractions. The greatest part of
labor is taken up by the first stage. The most important thing is the progress
of labor provided the woman is comfortable and the fetus is well. The labor
last longer in primigravidae than in multigravidae.
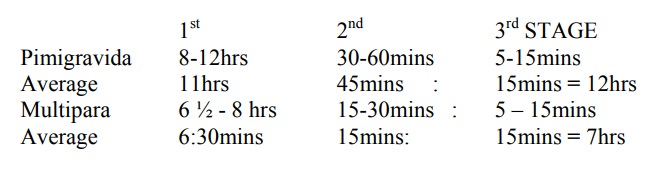
Some
times primigravidae spend less time while multipara spend more time in labour.
Evidences have shown that the use of Oxytocin and one-to-one care has reduced
the period of labour considerably.
Calculation of duration of labour
Example:
Date –
12/6/2008
Time:
Labour
begins – 12:30a.m
OS fully
dilated – 7.15a.m
Baby
delivered – 7.25am.
Placenta
& membranes delivered – 7.38a.m 1st Stage: 12.30 – 7.15a.m =
6hrs : 45mins
2ndStage
: 7.15 – 7.25a.m = 10mins
3rd
Stage: 7.25 – 7.33a.m = 8mins
TOTAL = 7hrs: 3mins
Physiology of labour
This
refers to the changes that take place during labor.
Contraction
This is
shortening of muscle fibre. Uterine contractions are involuntary, peristaltic
and intermittent. They are regular and painful in nature, enough to distract
patient from her normal activities. They are controlled by nervous system and
endocrine influence. Normal contractions increase in frequency, strength and
duration. They become more painful, rhythmic in nature, starts by occurring
every 15-20 minutes in early labor (frequency) and increase to 2-3 minute in
second stage, strength increases in intensity lasting 50-60 second in duration
at the end of first stage. The pain of contraction has the same characteristic
as that of spasmodic dysmenorrhea. It compresses the gestational sac and raises
the intrauterine pressure from about 5-10 mmHg to 25mmHg in labor and even
increases to 50-75mmHg at the height of contractions in the second stage of
labour. As a result pressure is directed towards the less resistant lower
uterine segment. This permit the cervix to dilate and the strongly contracting
fundus to expel the fetus in the second stage.
Fundal Dominant
Each
contraction starts at the fundus near the cornua and spread gradually across
downwards to the lower uterine segment, but usually remain stronger and last
longer at the upper region of the uterus (fundus), but the peak is reached
simultaneously over the whole uterus and the contraction fades from all part
together.
Retraction
Retraction
is peculiar to the uterine muscles only, whereby the wave of contraction does
not pass off entirely, but the musclefibres retain some of the contractile tone
instead of relaxing completely. Retraction assists in the progressive expulsion
of the fetus by maintaining the downward pressure. As the upper uterine segment
becomes shorter, thicker and the cavity reduces the lower uterine segment becomes
longer and thinner.
Polarity
This is
the neuro-muscular harmony that prevails between the upper and the lower
uterine segments. The two poles act harmoniously. The upper segment contracts
strongly and retracts to expel the fetus while the lower uterine segment
contract slightly and stretches to expel the fetus. If polarity is disorganized
the progress of labor is inhibited.
Formation of upper and lower uterine segment
By the
end of pregnancy the uterus divide into two distinct poles. The lower segment
develops from the isthmus, internal Os and the cervical canal. During labor the
retracted longitudinal fibres in the upper segment exert a pull on the lower
segment making it to stretch. This causes the Os to dilate and become part of
the lower segment. The upper segment is concerned with contraction and is
getting thicker while the lower segment which is for distention and dilatation
is getting thinner aided by the force of the descending head.
Development of retraction Ring: The ridge
which formswhere the thick upper segment meet the thin lower segment is known
as Retraction Ring. It is a normal ring and should not be felt or seen per
abdomen. When it becomes abnormal and can be seen or felt on palpation is known
as bandl’s ring . It is a sign of obstructed
labour when the upper segment is abnormally thick and the lower segment is
abnormally thin. It rises as the upper segment contracts and retracts until
full cervical dilatation.
Taking up of the Cervix Effacement: When
labour begins themuscle fibres surrounding the internal Os are drawn up by the
retraction of the upper uterine segment. The cervix becomes shortened as it
merges with the lower uterine segment. It takes place before dilatation in
primp but in multip it occurs as the cervixis dilating. In grande multiparae
complete effacement may not take place.
Dilatation of the cervix: Is the
widening of the external Os. Theretracted muscle fibres of the upper segment
exert a pull on the weak lower segment and the cervix, making, it to dilate
from a thing closed aperture to an opening large enough to permit passage of
the fetal head.
In
primigravida the internal Os dilates at the same time the cervix is being taken
up, and then the external OS dilates later. In the multiparous woman both the
internal and the external OS dilate as the cervix is being taken up. Dilatation
of the Os is a gradual process. Full dilatation is 10cm. A well flexed head
favours efficient dilatation.
Show
The lost
of blood stained mucoid discharge as the cervix dilate. It is from the plug of
mucus that guards the cervical canal during pregnancy. It can be seen a few
hours before or after labour has started.
Formation of bag of waters
When the
lower uterine segment stretches, the chorion get detached from it and the
increase intra uterine pressure causes the bag of fluid to bulge through the
dilating internal OS. The well flexed head which fix neatly into the cervix cut
off the fluid in front of the head from the one which surrounds the behind
body. This one in front is known as forewaters
and the behind is known as Hind –
waters
Advantage: It prevents transmission of
pressure from the hindwater from being applied on the fore water so keeps the
membranes intact during first stage of labour.
General Fluid Pressure:Is the
term used when the amniotic fluidequalizes the pressure throughout the uterus
during contractions. It ensures adequate supply of oxygen to the fetus during
contraction by preventing compression of the placenta by the fetus.
Rupture of Membranes: the
amniotic sac should remainintact until the OS is fully dilated (end of the 1st
stage) but this is not always the case. In badly fitting presenting part the
membranes rupture quite early because the fore waters are not cut off
completely from the hind waters so there is transmission of pressure to the
fore waters during the intra uterine contractions. In some cases it does
happens for no apparent reasons. Sometimes the membranes do not rupture even at
2nd stage and the baby is born with it, this is known as “caul”. Ruptured
membran e (RM) may be spontaneous or artificial – ARM. Artificial rupture of
membrane (ARM) promotes labour.
Physiology of the second stage
Contraction
and Retraction continue: During this stage the contraction are more severe,
stronger and expulsive, occurring more frequently (about 1-2mins) and of longer
duration about 60sec or more. The fetal head press and stretches the vagina
which in-turn stimulates uterine action. Also the membranes help the fetus to
be in close contact with the cervix, the upper segment gets much shorter and
thicker. The placental circulation is much more interfered with than during
first stage. The pain suffered during this time is less and different in
characteristic from that of first stage because the pain is due to stretching
of the vagina, pelvic and perineum. It is therefore felt in the back, pelvis
and may radiate down the inner surface of the thigh.
Secondary
powers come into play/Accessory muscle: the abdominal muscles and diaphragm now
come into play to help with the expulsive contractions to expel the fetus. The
woman now has the urge to push “known as bearing do wn”. As the presenting part
reaches the pelvic floor and descent it, the pushing becomes involuntary.
Secondary powers help to overcome the pelvic floor resistance.
Displacement
of the pelvic floor: This is a “swing door action.” The anterior wall of the
vagina and the pe lvic floor are pushed upwards and forwards while the
posterior wall of the vagina and pelvic floor push downwards and backwards.
The bladder
is drawn up into the abdominal cavity. The rectum is compressed by the
advancing head, anus bulges, defecation may take place and the anus gapes. The
perineal body stretches and thins out lengthen the posterior wall of the birth
canal causing the vaginal orifice to be directed upwards.
Expulsion
of the Fetus: With each contraction the head descends along the birth canal and
recedes in between contractions until it is seen on the vulva. This continues
until crowning takes place. When the head no longer recedes between
contractions the bi-parietal diameter distend the vaginal orifice and occiput
escapes under the symphysis pubis. The head is born by extension. The rest of
the body is born by lateral flexion and remaining liquor amni expelled.
Physiology of third stage
Contraction
and Retraction Continue: As the upper segment becomes thicker and smaller after
the birth of the baby the placenta site also become reduced this makes the
placenta to buckle off the uterine wall and separate. The placenta drops into
the lower uterine segment or the vagina, followed by the membranes which
stripped off the uterine wall by the traction of the descending placenta. The
stronger the contraction the sooner the placenta separates (5 mins) about 1/3
seprate with the birth of the baby.
Methods of placental separation
There are
two methods of separation and expulsion of the placenta.
Shultze Method: 80%: This is
the most common method. Inthis method separation starts from the centre of the
placenta and with the aid of Retroplacenta clot the placenta drop into the
lower uterine segment or into the vagina. During delivery the fetal surface
appears first at the vulva followed by the membranes. There is minimal blood
loss with this method. The 3rd stage is neat
Mathews Duncan Method 20%: In this
method separationstarts at the edge and slides down sideways. It comes through
the vulva
with the lateral border first, like a button through a button hole. The
maternal surface is seen first at the vulva. There is trickling of blood
throughout the third stage. The third stage .is messier.
Control of bleeding: the
Contraction and retraction of theuterine muscle fibers that bring about
separation of the placenta also act as “living Ligatures” by compress ing the
blood vessels and controlling the bleeding. The clothing mechanism is of little
value untill later when contractions are much less. The opposite wall are now
in contact and apply further pressure on the placenta site.
Related Topics