Chapter: Clinical Cases in Anesthesia : One-Lung Anesthesia
How is correct positioning of the double-lumen endobronchial tube assessed?
How is
correct positioning of the double-lumen endobronchial tube assessed?
Correct placement of the endobronchial tube
must be confirmed immediately after intubation and after turning the patient
into the lateral decubitus position. The patient’s lungs are initially
ventilated through both lumens with the tracheal cuff inflated. Bilateral
breath sounds, bilateral chest excursion, and bilateral fogging of
endobronchial tube lumens should be present. Gas should not leak around the
cuff. The capnogram should be examined for excretion of CO2.
Successful response to these maneuvers ensures that the distal end of the
tracheal lumen is in the trachea and is above the carina. Unilateral breath
sounds and chest movement indicate that the tube has been inserted too far, and
the tracheal lumen is in the bronchus, ipsilateral to the side on which breath
sounds are present. In this case, the tracheal cuff should be deflated and the
tube withdrawn until bilateral ventilation is established.
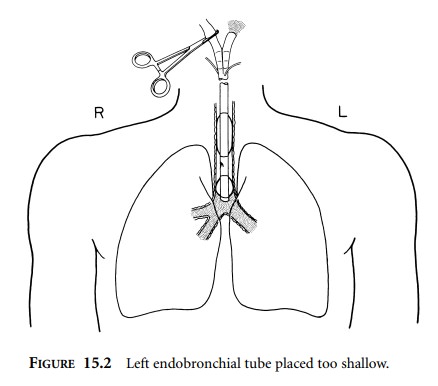
Next, the bronchial balloon is inflated with
less than 2 mL of air (Figure 15.1). The tracheal lumen is clamped and the
access cap opened. Ventilation should result in chest movement and breath
sounds on the endobronchial side. The presence of bilateral breath sounds and
chest movement indicates that the bronchial lumen’s orifice is proximal to the
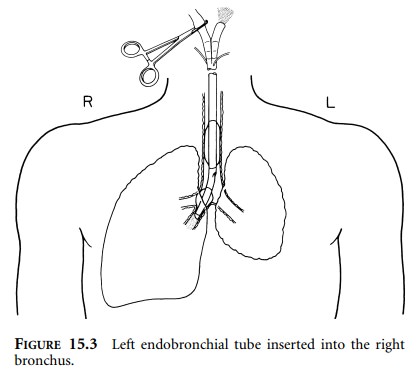
carina (Figure 15.2). Unilateral breath sounds and chest movement of the side
opposite the bronchus intended for intubation indicate that the tube has been
placed in the wrong side (Figure 15.3). If this has happened, both cuffs should
be deflated and the tube with-drawn to a point where the distal end of the
endobronchial tube is in the trachea. The tube is then rotated and advanced
again until there is resistance to further movement. An alternative method is
to insert a fiberscope through the bronchial lumen, visualize the carina, pass
the fiberscope down the bronchus intended for intubation, and then slide the
tube distally using the fiberscope as a guide until resist-ance is met. If the
trachea was easy to intubate, instead of remanipulating the tube within the
patient, the tube can be removed from the patient entirely, and the procedure
repeated. A right-sided tube will almost always go to the right side, but a
left-sided tube will sometimes pass to the right side. A left-sided tube should
not be allowed to remain in the right side, because there is no opening for the
right upper lobe bronchus on a left-sided tube. Rotating
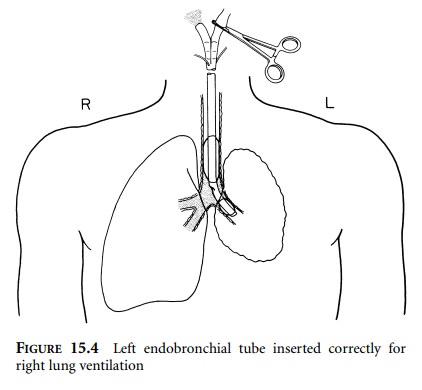
Ventilation of the lung while the endobronchial
lumen is clamped should provide breath sounds and chest move-ment only on the
side opposite the bronchus intended for intubation, provided the tube has been
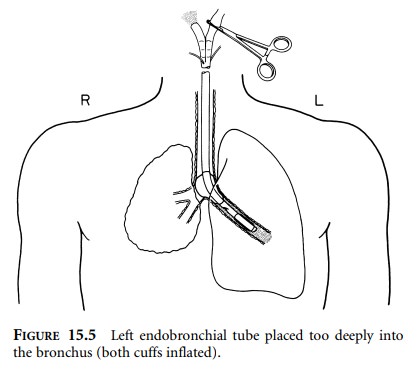
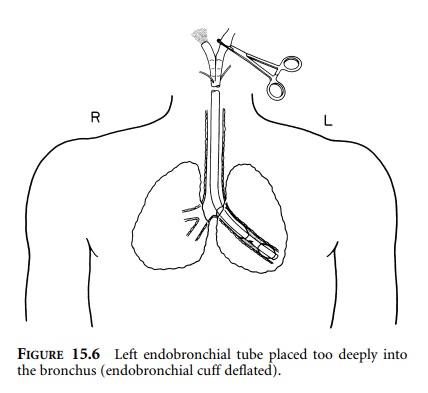
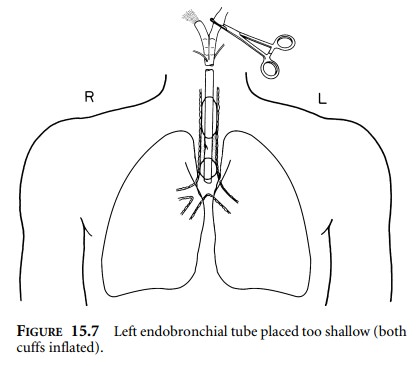
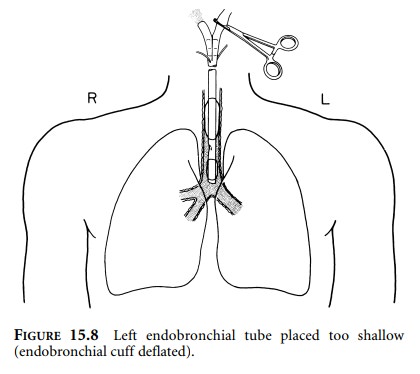
placed in the appropriate bronchus (Figure 15.4). Inability to ventilate during
this maneuver indicates that the tube has been malpositioned and is either too
deep in the bronchus or too shallow in the trachea. Deflation of the
endobronchial cuff while keeping the endobronchial lumen clamped will allow
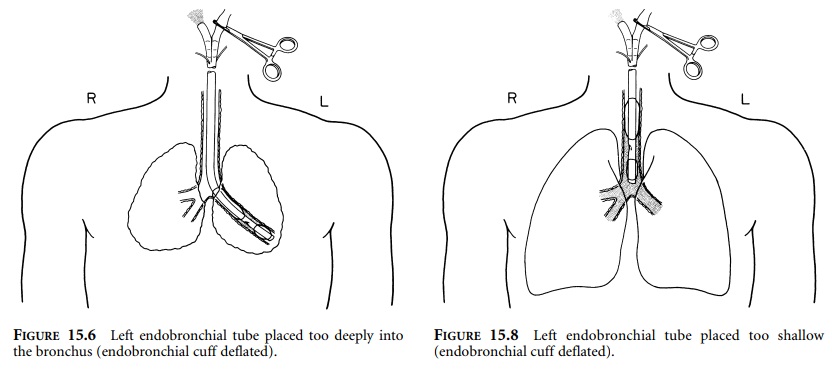
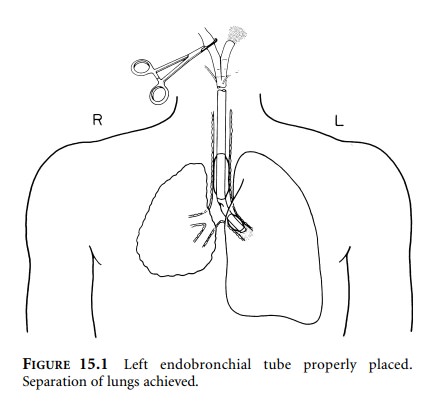
ventilation of only one lung if the tube is too deep in the bronchus (Figures
15.5 and 15.6), or bilateral lung ventilation if the tube is too shallow in the
trachea (Figures 15.7 and 15.8). Ventilation of the lung contralateral to the
position of the endobronchial lumen and only the upper lobe of the side
ipsilateral to endobronchial tube placement indicates that the cuff of the
endobronchial tube is distal to the upper lobe bronchus and that the tube needs
to be withdrawn.
The precise positioning of the tube can be
evaluated with the use of a flexible fiberoptic bronchoscope. Passage down the
tracheal lumen should reveal the carina and just the proximal tip of the blue
cuff of the bronchial lumen at
Visualization of the tube passing into the bronchus beyond the carina without
observation of the blue bronchial cuff indicates that the tube is positioned
too deep into the bronchus. Inspection via the bronchial side should reveal a
patent bronchial lumen that is not occluded internally by the cuff. If the
tube’s distal opening opposes the bronchial wall, ventilation of that lung
becomes difficult because double-lumen tubes lack Murphy eyes. Visualization of
the bronchial carina indicates that the tube is not placed too deeply. If the
tube is right-sided, visualization through the side opening should allow proper
alignment with the right upper lobe bronchus. If, after placing a fiberscope
through the tracheal lumen, the carina is not visualized, the tube is probably
too shallow, too deep, or located in the unintended bronchus. If the tube is
too shallow, then defla-tion of the bronchial balloon should provide a view of
the carina. If the tube is down the contralateral bronchus, then deflation of
the bronchial cuff will not demonstrate tracheal carina, but opposite side
anatomy will be observed. For example, if a left-sided tube lodges in the right
bronchus, then deflation of the bronchial cuff will demonstrate bronchus
intermedius (right upper lobe, right middle lobe, and right lower lobe
bronchi).
Related Topics