Chapter: Clinical Cases in Anesthesia : Antagonism of Nondepolarizing Neuromuscular Blockade
Explain the need for antimuscarinics used in conjunction with acetylcholinesterase inhibitors
Explain
the need for antimuscarinics used in conjunc-tion with acetylcholinesterase
inhibitors.
Inhibitors of acetylcholinesterase cause a
dramatic increase in the concentration of acetylcholine at all effector organs.
While this improves neuromuscular transmission by acting on the nicotinic
receptor of the neuromuscular junction, increased acetylcholine concentration
has many undesirable effects on visceral end-organs. These effects are mediated
by the muscarinic subset of acetylcholine recep-tors. Atropine and
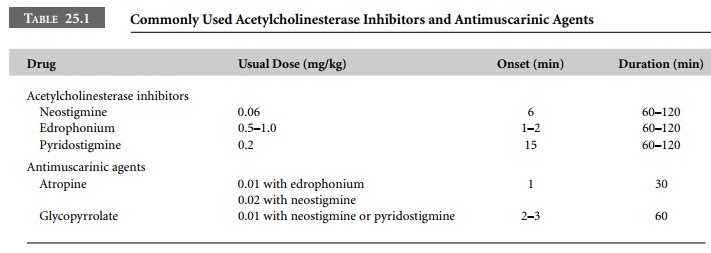
glycopyrrolate are used to prevent these muscarinic effects (Table 25.1).
The most dramatic and feared muscarinic effect
is that on the heart. Acetylcholinesterase inhibitors may cause profound
bradycardia, nodal or ventricular escape beats, or even asystole. Increased
gastrointestinal motility with excess salivation and diarrhea are other
undesirable effects.
The pulmonary system is profoundly affected as
well, with increased airway secretions and bronchospasm causing wheezing and
difficulty in ventilation.
To prevent these undesirable side-effects,
acetyl-cholinesterase inhibitors are given with an antimuscarinic agent, either
atropine or glycopyrrolate. Administration of these agents together with
acetylcholinesterase inhibitors prevents life-threatening bradydysrhythmias and
limits airway secretions, avoiding ventilatory problems.
Because the onset time of atropine is more
rapid than that of glycopyrrolate, it is frequently used in combination with
edrophonium. Atropine 0.01 mg/kg should precede the administration of
edrophonium. Once a tachycardia occurs, appropriate doses of edrophonium may be
given. This ensures that atropine’s vagolytic effects precede the vagotonic
(bradycardic) effects of edrophonium. Atropine, 0.02 mg/kg, may be combined
with or precede the admin-istration of neostigmine. This may result in
tachycardia, however, because atropine has a more rapid onset than neostigmine.
Glycopyrrolate, with a slower onset than atropine, is usually administered
together with neostigmine, providing offsetting chronotropic stability.
Neostigmine and glycopyrrolate may be given separately or combined in a single
syringe. The latter approach, while generally safe, should not be used in
patients with conduction defects or sick sinus syndrome, because
life-threatening bradycardia may result. Occasionally, patients who do not
demonstrate a tachycardic response to antimuscarinics are encountered. These
patients should not receive acetylcholinesterase inhibitors unless a
functioning pacemaker is available. Alternatively, neuromuscular muscle
relaxants may be allowed to wear off spontaneously.
Related Topics