Chapter: Psychiatric Mental Health Nursing : Schizophrenia
Etiology - Schizophrenia
ETIOLOGY
When question for researchers and clinicians for as long as they
have studied the illness. In the first half of the 20th cen-tury, studies
focused on trying to find a particular patho-logic structure associated with
the disease, largely through autopsy. Such a site was not discovered. In the
1950s and 1960s, the emphasis shifted to examination of psychologi-cal and
social causes. Interpersonal theorists suggested that schizophrenia resulted
from dysfunctional relation-ships in early life and adolescence. None of the
interpersonal theories has been proved, and newer scientific studies are
finding more evidence to support neurologic/neurochemi-cal causes. However,
some therapists still believe that schizophrenia results from dysfunctional
parenting or family dynamics. For parents or family members of per-sons
diagnosed with schizophrenia, such beliefs cause agony over what they did
“wrong” or what they could have done to help prevent it.
Newer scientific studies began to demonstrate that schizophrenia
results from a type of brain dysfunction. In the 1970s, studies began to focus
on possible neurochemi-cal causes, which remain the primary focus of research
and theory today. These neurochemical/neurologic theories are supported by the
effects of antipsychotic medications, which help to control psychotic symptoms,
and neuroimag-ing tools such as computed tomography, which have shown that the
brain of people with schizophrenia differs in struc-ture and function from the
brain of control subjects.Whether schizophrenia is an organic disease with
under-lying physical brain pathology has been an important question for
researchers and clinicians for as long as they have studied the illness. In the
first half of the 20th cen-tury, studies focused on trying to find a particular
patho-logic structure associated with the disease, largely through autopsy.
Such a site was not discovered. In the 1950s and 1960s, the emphasis shifted to
examination of psychologi-cal and social causes. Interpersonal theorists
suggested that schizophrenia resulted from dysfunctional relation-ships in
early life and adolescence. None of the interpersonal theories has been proved,
and newer scientific studies are finding more evidence to support
neurologic/neurochemi-cal causes. However, some therapists still believe that
schizophrenia results from dysfunctional parenting or family dynamics. For
parents or family members of per-sons diagnosed with schizophrenia, such
beliefs cause agony over what they did “wrong” or what they could have done to
help prevent it.
Newer scientific studies began to demonstrate that schizophrenia
results from a type of brain dysfunction. In the 1970s, studies began to focus
on possible neurochemi-cal causes, which remain the primary focus of research
and theory today. These neurochemical/neurologic theories are supported by the
effects of antipsychotic medications, which help to control psychotic symptoms,
and neuroimag-ing tools such as computed tomography, which have shown that the
brain of people with schizophrenia differs in struc-ture and function from the
brain of control subjects.
![]()
![]()
Biologic Theories
The biologic theories of schizophrenia focus on genetic factors,
neuroanatomic and neurochemical factors (struc-ture and function of the brain),
and immunovirology (the body’s response to exposure to a virus).
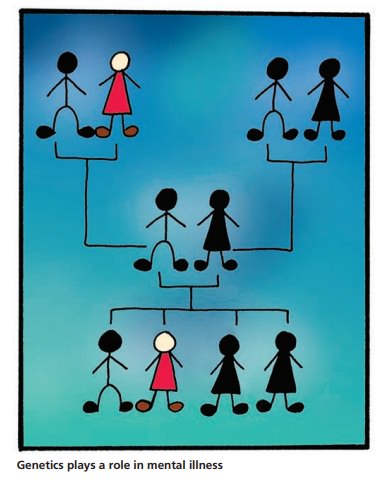
Genetic Factors
Most genetic studies have focused on immediate families (i.e.,
parents, siblings, and offspring) to examine whether schizophrenia is
genetically transmitted or inherited. Few have focused on more distant
relatives. The most important studies have centered on twins; these findings
have demon-strated that identical twins have a 50% risk for schizophre-nia;
that is, if one twin has schizophrenia, the other has a 50% chance of
developing it as well. Fraternal twins have only a 15% risk (Kirkpatrick &
Tek, 2005). This finding indicates that schizophrenia is at least partially
inherited.
Other important studies have shown that children with one biologic
parent with schizophrenia have a 15% risk; the risk rises to 35% if both
biologic parents have schizophre-nia. Children adopted at birth into a family
with no history of schizophrenia but whose biologic parents have a history of
schizophrenia still reflect the genetic risk of their biologic parents. All
these studies have indicated a genetic risk or tendency for schizophrenia, but
genetics cannot be the only factor: identical twins have only a 50% risk even
though their genes are 100% identical (Riley & Kendler, 2005).
Neuroanatomic and Neurochemical Factors
With the development of noninvasive imaging techniques such as
computed tomography, magnetic resonance imag-ing, and positron emission
tomography in the past 25 years, scientists have been able to study the brain
structure (neu-roanatomy) and activity (neurochemistry) of people with
schizophrenia. Findings have demonstrated that people with schizophrenia have
relatively less brain tissue and cerebrospinal fluid than those who do not have
schizophre-nia (Schneider-Axmann et al., 2006); this could represent a failure
in the development or a subsequent loss of tissue. Computed tomography scans
have shown enlarged ventri-cles in the brain and cortical atrophy. Positron
emission tomography studies suggest that glucose metabolism and oxygen are
diminished in the frontal cortical structures of the brain. The research
consistently shows decreased brain volume and abnormal brain function in the
frontal and temporal areas of persons with schizophrenia. This pathol-ogy
correlates with the positive signs of schizophrenia (temporal lobe), such as
psychosis, and the negative signs of schizophrenia (frontal lobe), such as lack
of volition or motivation and anhedonia. It is unknown whether these changes in
the frontal and temporal lobes are the result of a failure of these areas to
develop properly or if a virus, trauma, or immune response has damaged them.
Intrauter-ine influences such as poor nutrition, tobacco, alcohol, and other
drugs, and stress also are being studied as possiblecauses of the brain
pathology found in people with schizo-phrenia (Buchanan & Carpenter, 2005).
Neurochemical studies have consistently demonstrated alterations in
the neurotransmitter systems of the brain in people with schizophrenia. The
neuronal networks that transmit information by electrical signals from a nerve
cell through its axon and across synapses to postsynaptic recep-tors on other
nerve cells seem to malfunction. The trans-mission of the signal across the
synapse requires a complex series of biochemical events. Studies have
implicated the actions of dopamine, serotonin, norepinephrine, acetyl-choline,
glutamate, and several neuromodulary peptides.
Currently, the most prominent neurochemical theories involve
dopamine and serotonin. One prominent theory suggests excess dopamine as a
cause. This theory was devel-oped based on two observations: First, drugs that
increase activity in the dopaminergic system, such as amphetamine and levodopa,
sometimes induce a paranoid psychotic reac-tion similar to schizophrenia.
Second, drugs blocking post-synaptic dopamine receptors reduce psychotic
symptoms; in fact, the greater the ability of the drug to block dopamine
receptors, the more effective it is in decreasing symptoms of schizophrenia
(Buchanan & Carpenter, 2005).
More recently, serotonin has been included among the leading
neurochemical factors affecting schizophrenia. The theory regarding serotonin
suggests that serotonin modu-lates and helps to control excess dopamine. Some
believe that excess serotonin itself contributes to the development of
schizophrenia. Newer atypical antipsychotics, such as clozapine (Clozaril), are
both dopamine and serotonin antagonists. Drug studies have shown that clozapine
can dramatically reduce psychotic symptoms and ameliorate the negative signs of
schizophrenia (Kane & Marder, 2005).
Researchers also are exploring the possibility that schizophrenia
may have three separate symptom com-plexes or syndromes:
hallucinations/delusions, disorgani-zation of thought and behavior, and
negative symptoms (Buchanan & Carpenter, 2005). Investigations show that
the three syndromes relate to neurobiologic differences in the brain. It is
postulated that schizophrenia has (these three) subgroups, which may be
homogeneous relative to course, pathophysiology, and, therefore, treatment.
Immunovirologic Factors
Popular theories have emerged stating that exposure to a virus or
the body’s immune response to a virus could alter the brain physiology of
people with schizophrenia. Although scientists continue to study these
possibilities, few findings have validated them.
Cytokines are chemical messengers between immune cells, mediating
inflammatory and immune responses. Specific cytokines also play a role in
signaling the brain to produce behavioral and neurochemical changes needed in
the face of physical or psychological stress to maintain homeostasis. It is
believed that cytokines may have a role in the development of major psychiatric
dis-orders such as schizophrenia (Brown, Bresnahan, & Susser, 2005).
Recently, researchers have been focusing on infections in pregnant
women as a possible origin for schizophrenia. Waves of schizophrenia in
England, Wales, Denmark, Finland, and other countries have occurred a
generation after influenza epidemics. Also, there are higher rates of
schizophrenia among children born in crowded areas in cold weather, conditions
that are hospitable to respiratory ailments (Brown, Bresnahan, & Susser,
2005).
Related Topics