Chapter: Essentials of Psychiatry: Ethnic and Cultural Perspectives in Psychopharmacology
Ethnic and Cultural Perspectives in Psychopharmacology
Ethnic and Cultural Perspectives
in Psychopharmacology
Dispelling the “Color Blind” Approach
Substantial
individual variation in drug responses, at times up to 100-fold in terms of
optimal dosing, is the rule rather than the ex-ception. Although the current
understanding of such remarkable variability remains incomplete, it is clear
that the interplay between genetics and environmental factors plays a pivotal
role in pharma-cotherapeutic responses, particularly in the context of an
individu-al’s ethnic origin, lifestyle and other socio-demographic variables.
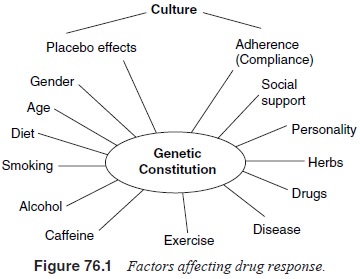
As shown
in Figure 76.1, virtually all factors affecting phar-macological responses are
significantly influenced by culture and ethnicity. Furthermore, patterns of
genetic polymorphism, often with substantial ethnic variation, exist in a large
number of genes encoding drug metabolizing enzymes as well as receptors and
transporters believed to be targets of pharmaceutical agents. The expression of
these genes is often significantly modified by a large number of environmental
factors, including diet and exposure to various substances (e.g., tobacco). Of
even greater importance, the success of any therapy, including pharmacotherapy,
depends on the participation of the patient and, as such, depends
signifi-cantly on the quality of interaction between the clinician and the
patient. The importance of culture in this regard is paramount.
Clinicians’ Attitudes
A large
body of literature indicates that patients’ cultural/ethnic backgrounds
significantly determine the way clinicians concep-tualize and label their
problems, which in turn dictate the choices for therapeutic intervention
(Mezzich et al., 1995). Using case
vignettes that are identical except for ethnic group identification, a number
of studies demonstrated that cases identical in every other aspect were
nevertheless given significantly more severe diagnoses if the patients were
identified as being of ethnic minor-ity origin (Gaw, 1993; Lopez, 1989).
Paralleling such a tendency, African-American psychiatric patients are more
likely to have been given a diagnosis of schizophrenia as compared with their
Caucasian counterparts (Littlewood, 1992; Lopez, 1989). Inter-estingly, in
studies where patients were reassessed with the use of structured interviews,
such differences largely disappeared, suggesting that such a differential
diagnostic pattern is possibly determined by variables related to clinicians’
biases rather than to the patients’ clinical conditions (Adebimpe, 1981;
Marquez et al., 1985; Mukherjee et al., 1983; Roukema et al., 1984).
Adherence
Most
studies exploring correlates of nonadherence have focused on patient and
treatment variables, and have shown that a large number of factors
significantly predict problems with adherence. These include the
sociodemographics of the patient, the financial burden of the treatment, and
the side effect profile of the medica-tions (Manne, 1998; Fenton et al., 1997). The health belief model
has served as the theoretical framework for a large number of seminal research
endeavors, which in aggregate demonstrate that the beliefs held by patients and
those significant in their lives to a large extent determine their
participation in and response to treatment decisions (Hughes et al., 1997).
Following
the logic of the health belief model, one would expect adherence to be an even
larger problem in cross-cultural clinical situations. This has been
substantiated by a number of clinical observations and reports of the service
utilization of particular ethnic minority groups (Sue et al., 1991). Compared with Caucasians, ethnic minority patients
are often found to en-ter treatment at a significantly delayed stage, and they
also are more likely to drop out of psychiatric treatment prematurely. Programs
aiming at bridging cultural gaps have been shown sig-nificantly to improve
treatment retention and outcome (Acosta et
al., 1982).
Adverse
effects of psychotropics are often substantial. De-pending on beliefs and
expectations, many positive drug effects could be interpreted either as
negative or positive. For example, in a study of Hong Kong Chinese bipolar
patients treated with lithium, Lee and colleagues (1992) found that, unlike
Western patients, the Chinese rarely complained of “missing the highs”, and
“loss of creativity” and actually regarded polydipsia, polyuria and weight gain
as part of the therapeutic effect of the medicine. In contrast, lethargy,
drowsiness and poor memory represented serious concerns for many of these
patients, and were promi-nent in their complaints, even though objectively they
were not likely to be due to the medications they were taking, since they
occurred at similar rates among matched controls. Such findings highlight the
importance of culturally based beliefs and expecta-tions in determining how
physical and psychological experiences associated with drug treatment and
recovery are attributed.
The Explanatory Model (EM) approach, as originally pro-posed by Kleinman (1988), may be a particularly effective way for the systematic assessment of such beliefs and expectations. By methodically eliciting the patient’s perspectives on the symptoms that are most salient and worrisome to them (patterns of distress), their attributions (perceived causes), their help-seeking experi-ences and preference, as well as their perception on stigma, dis-crepancy between the patients’ and the professionals’ EMs could be systematically identified and bridged (Weiss, 1997). Elements of the EM are included in Appendix I of the DSM-IV manual as part of the Outline for Cultural Formulation (American Psychiat-ric Association, 1994).
Expectation (“Placebo”) Effects
The term
“expectations effect” reflects the importance and power of expectation and
beliefs on treatment effects in deter-mining patients’ response to any therapy,
whether psychoso-cial or pharmacological. Expectations regarding the safety and
effectiveness of any therapeutic interventions, in turn, are shaped by
patients’ sociocultural backgrounds as well as individual “idi-osyncratic”
experiences (e.g., past experiences of side effects). Since patients’ beliefs
regarding medical treatments are often shaped by their cultural backgrounds, it
stands to reason that pa-tients’ expectation regarding the therapeutic effect
of the offered treatment would be largely affected by their cultural construct
of the illness.
Despite
rapid modernization, traditional medical theo-ries and practices remain deeply
rooted and influential in de-termining individuals’ health beliefs and
behaviors in many so-cieties (Wolffers, 1989; Okpaku, 1998; Wig, 1989;
Rappaport, 1977). For example, most traditional medical systems em-phasize the
importance of maintaining a dynamic balance between “coldness” and “hotness”
(Castro et al., 1994) or be-tween
“Yin” and “Yang” in the case of the Chinese system (Lin, 1981). These
principles provide guidance for assessment as well as for formulating treatment
approaches. For patients who subscribe to such beliefs, a perceived mismatch
between the therapeutic agents and the afflictions may significantly lower the
expectation effect. For example, red-colored pills might be regarded as capable
of enhancing the “hot” element, and might be regarded as less effective in the
treatment of con-ditions perceived as a result of excessive “hotness” (e.g.,
fever, anxiety state, or mania). Interestingly, Buckalew and Coffield (1982)
reported findings from a well-controlled study showing significant ethnic
differences in response to placebo pills with different colors.
The Concomitant Use of Alternative/ Indigenous Treatment and Healing Methods
“Alternative”
health care traditions (e.g., Chinese medicine and Ayurvedic medicine) seemed
to have responded well to chal-lenges of modern medicines and have continued to
evolve and thrive (Landy, 1977; Leslie, 1976). Multiple medical and heal-ing
traditions and treatment modalities coexist in all socie-ties, and patients
often utilize these services simultaneously or sequentially, frequently without
informing their physicians. Problems with drug–drug interactions from such
behavior that could potentially arise from such a practice are not limited to
particular ethnic groups, and constitute an important considera-tion for
clinicians prescribing medications.
Various
herbs utilized by traditional practitioners and healers are biologically active
(it has been estimated that approxi-mately 40% of our “modern”
pharmacotherapeutic agents origi-nated from natural sources [Balick and Cox,
1996]). Although much remains unclear, herbal preparations do exert significant
impact on various biological systems, including those crucial for the
functioning of the central nervous system (Cott, 1997; Duke, 1995). Since most
patients do not regard herbs as medi-cines and typically fail to inform their
physicians of such uses unless specifically inquired, toxicities or treatment
failures due to “herb–drug interactions” are likely widespread and
unsus-pected. Herbal preparations may modulate the effect of modern therapeutic
agents, including psychotropics, both at the pharma-codynamic level (the effect
of the drugs on the organism), and at the pharmacokinetic level.
Biological Diversity and Its Consequence in Psychotropic Responses
Emerging
data now convincingly demonstrate that for the ma-jority of the genes,
polymorphism is the rule rather than the exception. Furthermore, the frequency
and distribution of alle-les responsible for such polymorphisms often vary
substantially across ethnic groups, effectively requiring that ethnicity always
be considered in genetic studies (National Institute of Mental Health, 1997).
These phenomena have long been known in blood and human lymphocyte antigen
(HLA) typing (Polednak, 1989). In recent years, it has become increasingly
clear that equally extensive polymorphisms exist in genes governing key aspects
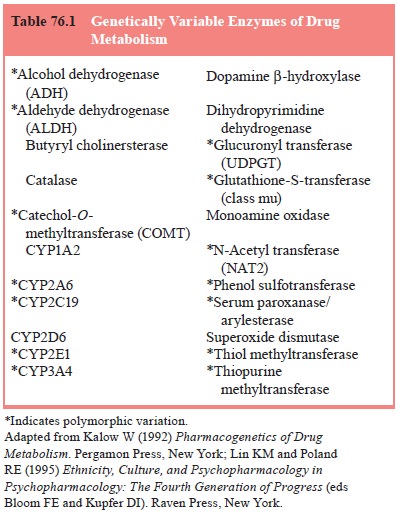
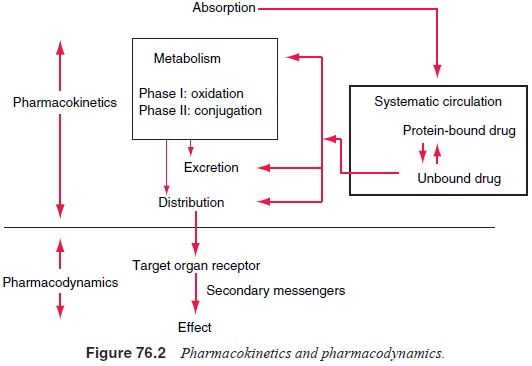
of how drugs are metabolized (see Table 76.1) as well as how they affect the
target organs. These processes, commonly called pharmacokinetics and
pharmacodynamics, are depicted in Figure 76.2 (Greenblatt, 1993). Together,
these genetic fac-tors may explain to a large extent the often extensive inter-indi-vidual
cross-ethnic variations in drug responses (Kalow, 1992; Lin et al., 1993).
Genetic Polymorphism of Genes Encoding “Drug-metabolizing Enzymes”: The Cytochrome P-450 System
As shown in Figure 76.2, of the four factors (absorption, distri-bution, metabolism and excretion) that together determine the fate and disposition of most drugs, variability in the process of metabolism is most substantial and usually is the reason for in-ter-individual and cross-ethnic variation in drug responses (Lin and Poland, 1995). Most drugs are metabolized via two phases: Phase I, commonly mediated by one or more of the cytochrome P-450 enzymes (CYPs), leads to the oxidation of the substrate; Phase II involves conjugation and is usually mediated by one of the transferases. There is clear evidence of inter-individual and cross-ethnic variations in the activity of enzymes in both phases, the genetic basis of which has been increasingly elucidated in recent years (Kalow, 1992; Weber, 1997).
Table
76.2 includes a list of major CYPs that are responsi-ble for the Phase I
metabolism of commonly used psychotropics
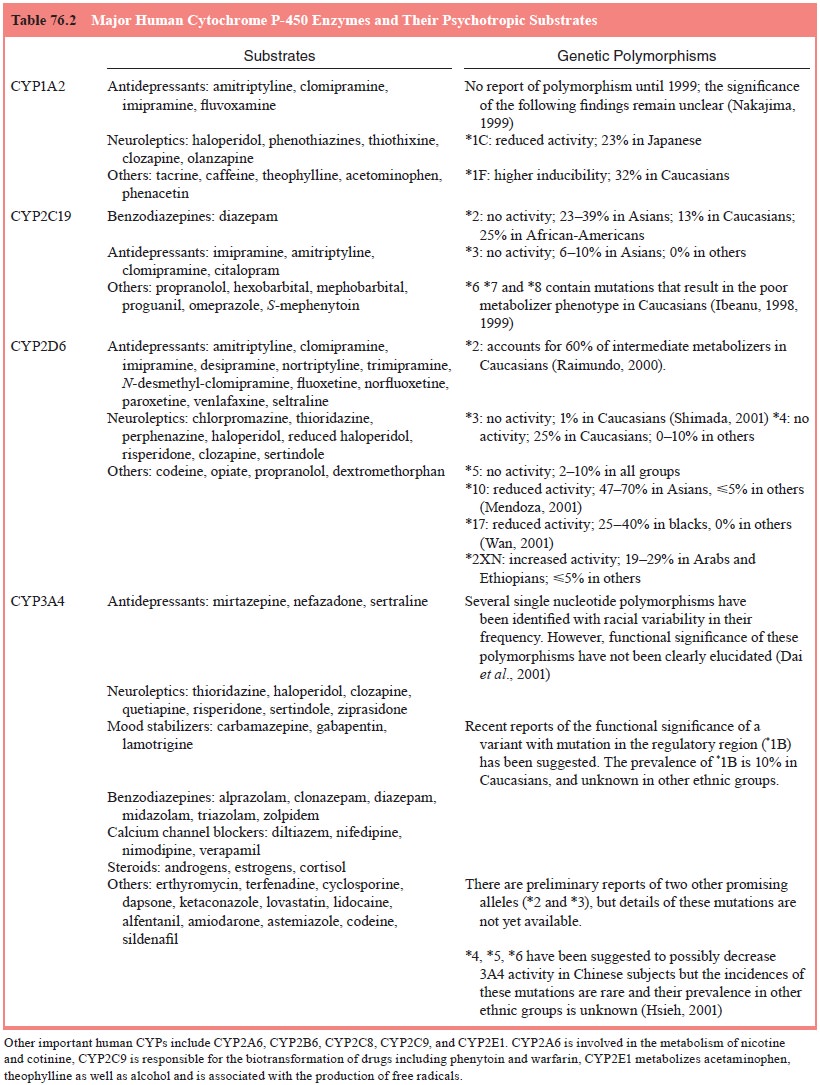
as well
as selected substances that are psychoactive and are com-monly used by
psychiatric patients.
Functionally
significant genetic polymorphisms exist in most of the CYPs (Lin and Poland,
1995), leading to extremely large variations in the activity of these enzymes
in any given population (Table 76.2). CYP2D6 represents the most dramatic
example, with more than 20 mutations that inactivate, impair, or accelerate its
function (Daly et al., 1996).
Significantly, most of these mutant alleles are to a large extent ethnically
specific.
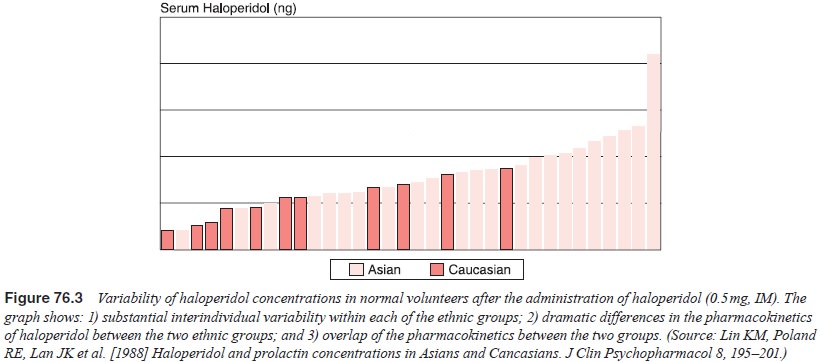
For
example, CYP2D6*4, which leads to the production of defective proteins, is
found in approximately 25% of Caucasians, but is rarely identified in other
ethnic groups. This mutation is mainly responsible for the poor metabolizers
(PM) in Caucasians (5–9%), who are extremely sensitive to drugs metabolized by
CYP2D6. Instead of CYP2D6*4, extremely high frequencies of CYP2D6*17 (Leathart et al., 1998, Masimirembwa and Hasler,
1997) and CYP2D6*10 (Wang et al.,
1993; Dahl et al., 1995; Roh et al., 1996) were found among those of
African and Asian ori-gins, respectively. Both of these alleles are associated
with lower enzyme activities and slower metabolism of CYP2D6 substrates (Figure
76.3), and may be in part responsible for previous find-ings of slower
pharmacokinetic profiles and lower therapeutic dose ranges observed in Asians
in regard to both classes of psy-chotropics, and in African-Americans in regard
to tricyclic anti-depressants (Lin and Poland, 1995).
Genetic
polymorphism also exists in CYP2C19, CYP2C9, CYP2E1, CYP3A4 as well as the
majority of other drug me-tabolizing enzymes. It is interesting to note that,
almost without exception, wherever genetic polymorphism is identified, the
al-lele frequency of the mutations typically show substantial ethnic variations
(Stephens et al., 1994; Gill et al., 1999; Kidd et al., 1999).
Patients
from different ethnic/cultural backgrounds live divergent lifestyles, and are
likely to be exposed to unique sub-stances that may have strong effects on the
expression and ac-tivity of drug metabolizing enzymes. Thus, what we currently
know about environmental influences on drug metabolism may represent only the
tip of the iceberg. This may be especially true in regard to ethnic minority
and other nonWestern populations.
For
example, studies have shown that Asian Indians and Afri-cans were significantly
slower in metabolizing substrates of CYP1A2, such as theophylline, antipyrine
and clomipramine. However, after they immigrated to Europe and adapted to the
new dietary habits, their metabolic profiles for these drugs became
indistinguishable from the “native” Westerner’s (Allen et al., 1977).
Genetic Polymorphism of Genes Encoding Receptors, Transporters, or Other Therapeutic Targets
Along
with the cloning and sequencing of the genes encoding the receptors and
transporters that mediate and regulate the function of important
neurotransmitters, it has become appar-ent that, contrary to earlier
predictions (Kalow, 1990), these genes are almost without exception highly
polymorphic, and the pattern of these polymorphisms vary significantly across
ethnicity (Gelenter et al., 1997;
Goldman et al., 1996; Hodge, 1994;
Dean et al., 1994; Chang et al., 1996). For example, the
frequency of the TaqI A RFLP polymorphism of the dopamine D2
receptor (DRD2), one of the most extensively investigated brain receptors,
ranges from 5 to 18% in Caucasians to approx-imately 36% in African-Americans
and 37 to 42% in Asians (Blum et al.,
1995). Similarly, dramatic ethnic variations exist in the pattern of genetic
polymorphism of many other recep-tor and transporter genes. These include other
DRD2 muta-tions (Taq1 B, 311Ser/Cys and exon 8 A/G substitution), other
dopamine receptors such as DRD4 and DRD3 (Parsian et al., 1999; Sander et al.,
1995; Sullivan et al., 1998), the
dopamine transporter gene (DAT1; locus symbol SLC6A3) (Vanden-bergh et al., 1992), the serotonin transporter
gene (5-HTT), and a number of serotonin receptors (5-HT2A-1438 A/G
and 5-HT2A-102 T/C) (Greenberg et
al., 1998; Smeraldi et al., 1998;
Michaelovsky et al., 1999).
These
polymorphisms may have functional significance and hence might be associated
with the risk for psychopathology as well as the response to treatment
regimens. We await further research to confirm this possibility.
Related Topics