Chapter: Microbiology and Immunology: Applied Microbiology: Nosocomial Infections
Epidemiology of Hospital-Acquired Infections
Epidemiology of Hospital-Acquired Infections
Sources of Infections
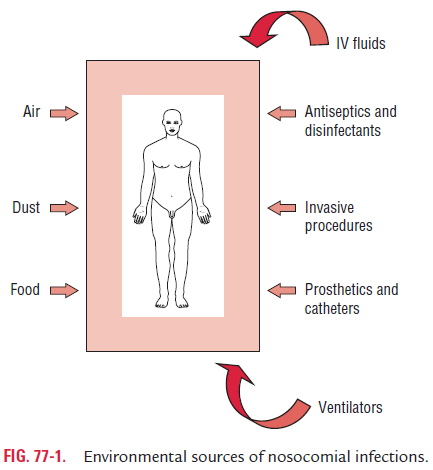
The sources of hospital-acquired infection may be exogenous or endogenous. Exogenous infection is most important and occurs mostly from (i) another patient, (ii) a member of the medical and paramedical staff harboring the pathogens, or (iii) from the environment. The latter includes inanimate objects, such as medical equipments (e.g., catheters, endoscopes, cystoscopes, etc.), bed pans, and surfaces contaminated by the patient’s secretions, excretions, blood, and other body fluids. It also includes hospital food, water, and environmental air (Fig. 77-1).
Endogenous infection is due to microbes present in thepatient’s own flora present in the body. Microorganisms from these floras may cause infections in different tissues of the patient during certain surgical operations, manipulation by instruments, or nursing procedures.
Microorganisms Causing Infections
Though initially much of the hospital outbreaks were caused by Gram-positive organisms like Streptococcus pyogenes and methicillin-resistant Staphylococcus aureus (MRSA), presently Gram-negative enteric pathogens including Escherichia coli,Klebsiella, Enterobacter species, etc., have emerged as an impor-tant cause of these infections.
Pseudomonas and Acinetobacter species are also common noso-comial pathogens, because they can survive as saprophytes in the environment and are extremely hardy, developing resistance to most of the commonly used antibiotics, and in some cases managing to grow even inside bottles of disinfectant solutions.
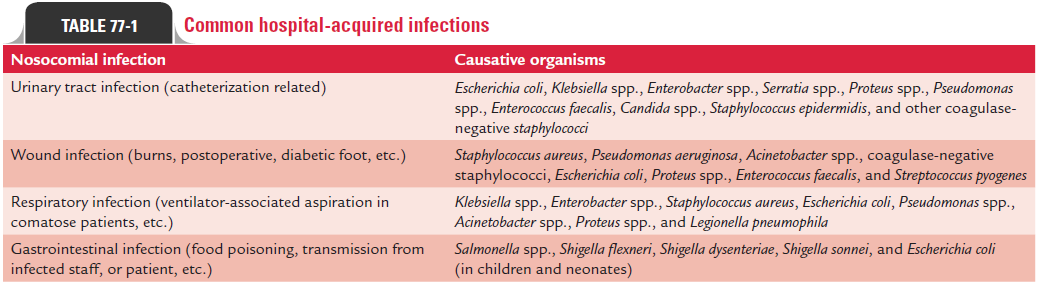
The microorganisms causing hospital-acquired infection are listed in Table 77-1.
There is also concern that these organisms may spread from hospitals into the general community—as evidence suggests that MRSA has done—especially into long-term care facilities, such as nursing homes, thereby causing a more serious health problem in the community.
Transmission of Infections
Many organisms gain entry to the body through breaches or evasion of “first line” body defenses. Breaches in epithelial inte-grity (e.g., surgical wounds, intravascular cannulas, and drain tubes), loss of the washing action of body fluids (e.g., because of a urinary catheter), and interference with first-line respiratory defenses (e.g., by anesthesia and endotracheal intubation) are common precursors of hospital-acquired infections. Infections can be transmitted by following ways.
◗ Air-borne transmission
Hospital infections may be transmitted by air-borne droplets, dust particles, and aerosols. Inhalation of air-borne droplets or droplets’ nuclei transmits Mycobacterium tuberculosis and many other respiratory pathogens. Hospital dusts generated from beddings, hospital floors, from skin by natural shed-ding of skin scales are rich sources of many pathogens, such as S. aureus, Pseudomonas aeruginosa,etc. Therefore, inhalation of these infective dust particles transmits infections. Aerosols produced by nebulizers, humidifiers, and air condition-ing apparatus transmit certain pathogen, such as Legionellapneumophila.
◗ Transmission by direct contact
Direct contact is the principal route of transmission of hospital-acquired infections. Direct contact with hands and clothings of medical personnel harboring microorganisms may transmit infection from one person to another. S. aureus and S. pyogenes are two important pathogens that are transmitted byhand contact. Certain pathogen, such as P. aeruginosa, can also be transmitted by contact with certain hospital instruments (e.g., endoscopes, bronchoscopes, cystoscopes, etc.) if not prop-erly disinfected.
◗ Transmission by oral route
Certain gastrointestinal pathogens may be transmitted by hos-pital foods served to hospitalized patients. The food may be the source of antibiotic-resistant P. aeruginosa, E. coli, Klebsiella spp., and other pathogens. These pathogens may colonize the intes-tine and later cause infection in the susceptible patients.
◗ Transmission by parenteral route
Blood-borne pathogens, such as hepatitis B and C and HIV (human immunodeficiency virus), may be transmitted by transfusion of blood or blood products, through contami-nated needles or sharp instruments that have not been properly disinfected.
Infections are also common among residents of long-term care facilities, such as nursing homes, special accommodation facilities, and rehabilitation hospitals. Predisposing factors include intrinsic patient factors (e.g., age and chronic medical conditions), presence of indwelling catheters, close communal living, immobility, incontinence, and frequent transfers back and forth between acute hospitals and the care facility. Urinary and respiratory tract infections and gastroenteritis are com-mon, and outbreaks of scabies have been described.ectio
Common Types of Hospital Infections
Common types of hospital infections can be grouped as follows:
◗ Urinary tract infections
Urinary tract infections (UTIs) account for as many as 40–45% of nosocomial infections. Although UTIs contribute only 10–15% to prolongation of hospital stay and to extra costs, these infections are important reservoirs and sources for spread of antibiotic-resistant bacteria in hospitals. Almost all noso-comial UTIs are associated with preceding instrumentation or indwelling bladder catheters, which create a 3–10% risk of infection each day.
The most common pathogens causing UTI are E. coli, noso-comial Gram-negative bacilli, enterococci, and Candida.
A patient who develops infection while the catheter is in place may complain of urethral discomfort, frequency, fever, and peri-catheter discharge. Infection occurring after catheter removal causes the usual symptoms of UTI. The presence of asymptomatic catheter-associated bacteriuria should not generally indicate a need for antimicrobial therapy. Possible exceptions include immunocompromised patients and patients undergoing uro-logical surgery. Asymptomatic catheter-associated candiduria often reflects vaginal or gastrointestinal carriage.
When symptoms are present, the catheter should be removed; if possible, a urine sample should be sent for culture, and a short course of antibiotic therapy should be given. If the urinary catheter must be kept in place, then antibiotic therapy may relieve the symptoms, but the organism is likely to per-sist. Prolonged antibiotic therapy in the presence of an indwell-ing catheter will result in the emergence of antibiotic-resistant organisms.n
◗ Nosocomial pneumonia
Nosocomial pneumonia accounts for 15–20% of nosocomial infections. Almost all cases of bacterial nosocomial pneumonia are caused by aspiration of endogenous or hospital-acquired oropharyngeal (and occasionally gastric) flora. Nosocomial pneumonias are associated with more deaths than are infec-tions at any other body site. The risk of dying from nosoco-mial pneumonia is affected greatly by many factors, including comorbidities, inadequate antibiotic treatment, and the involvement of specific pathogens (particularly P. aeruginosa and Acinetobacter). Surveillance and accurate diagnosis of pneumonia are often problematic in hospitals because many patients, especially those in the intensive care units (ICUs), have abnormal chest roentgenographs, fever, and leukocytosis potentially induced by many causes.pp
Early-onset nosocomial pneumonia, which manifests within the first 4 days of hospitalization, is most often caused by community-acquired pathogens, such as Streptococcus pneu-moniae and Haemophilus species. Late-onset pneumonia ismost commonly caused by S. aureus, P. aeruginosa, Enterobacter species, K. pneumoniae, or Acinetobacter species—the pathogens of increasing concern in many ICUs. Infection is polymicrobial in as many as 20–40% of cases.
The role of anaerobic bacteria in ventilator-associated pneumonia is not well defined. The appropriate duration of therapyfornosocomialpneumonia,althoughusuallyrangesfrom 10 to 21 days, is not well studied.
◗ Surgical wound infections
Surgical wound infections account for nearly 30% of all hospi-tal infections. These occur in up to 10% of patients undergoing clean surgery; the incidence varies with complexity of surgery, intrinsic patient risk, and surgical skills.
Most surgical wound infections result from contamination of the surgical wound with the patient’s own flora or that of operating-room personnel or environment at the time of the surgery. Postoperative hematogenous seeding of the wound site is uncommon.
The common clinical features of surgical wound infection are localized pain, redness, and discharge. Fever that occurs within 4 weeks of surgery, without other localizing features, is likely to be caused by infection at the surgical site. Superficial wound infection may resolve with or without antibiotics. Deeper or organ-space infection may require imaging for diag-nosis, surgical drainage, and antimicrobial therapy guided by culture of purulent material.
The likely causative organisms of surgical wound infections depend on the location and type of surgery. MRSA is most common cause in some hospitals. Gram-negative bacilli (e.g., E. coli) are more common causes of infection following gastro-intestinal or genitourinary tract surgery.
Related Topics