Chapter: Clinical Cases in Anesthesia : Myasthenia Gravis
Describe a reasonable anesthetic technique for a patient with MG undergoing transcervical thymectomy
Describe
a reasonable anesthetic technique for a patient with MG undergoing
transcervical thymectomy.
All patients undergoing anesthetic care should
have a continuous electrocardiogram, blood pressure, pulse oximeter, end-tidal
carbon dioxide, peripheral nerve stim-ulation (when relaxants are used or
weakness is antici-pated), and inspired oxygen monitoring. In general,
additional monitoring is dictated by surgical requirements and coexisting
disease. Induction of anesthesia follows denitrogenation with 100% oxygen and
proceeds with injection of a short-acting rapid-onset barbiturate, propo-fol,
or etomidate.
Tracheal intubation and controlled ventilation
are essen-tial in these patients. Muscle relaxation for tracheal intuba-tion is
often not required but may be facilitated by ventilation with potent inhalation
agents. If succinylcholine is used for rapid airway control, 2 mg/kg may be
required and can have a prolonged duration of action. Despite the
well-recog-nized resistance of myasthenics to succinylcholine, usual clinical
doses, which exceed 5 times the ED95, produce adequate relaxation
for endotracheal intubation, making dosing unpredictable. Some authors feel
that muscle relax-ants are best avoided in these patients, recommending that
potent inhaled agents will provide adequate relaxation for most procedures.
Some patients may not tolerate the cardiovascular depression associated with
these agents and may require a balanced technique with muscle relaxants. Small
incremental doses of intermediate-acting nondepolar-izing muscle relaxants may
be titrated with the assistance of peripheral nerve stimulation. Vecuronium,
cisatracurium, and mivacurium have short elimination half-lives and may not
require antagonism at the end of surgery.
Residual postoperative neuromuscular blockade
pres-ents another controversy. Some feel that continued ventila-tion until
adequate strength has returned is the safest management for these patients.
Others feel that anti-cholinesterases (with an antimuscarinic) may be titrated
in small doses to nerve stimulation response. Administration of excessive
amounts of an anticholinesterases risks cholin-ergic crisis. The decision to
antagonize residual postopera-tive neuromuscular blockade must be
individualized, and the risk of cholinesterase inhibitors (cholinergic crisis,
bradydysrhythmias, and increased secretions) must be weighed against the risk
of postoperative ventilation. Respiratory distress may be treated intravenously
with 1/30th of the usual oral pyridostigmine dose.
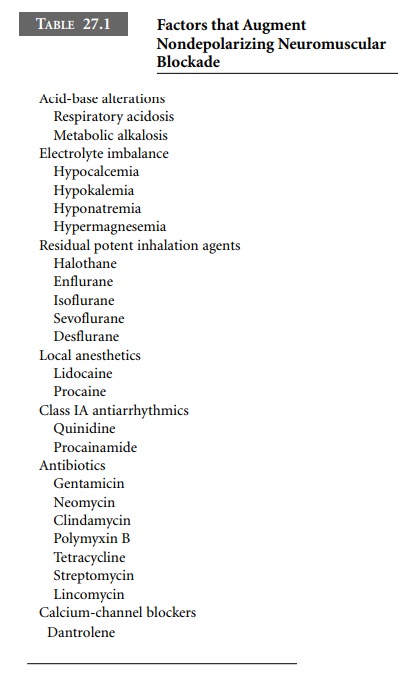
Other factors with slight neuromuscular
blocking prop-erties can take on additional importance in the face of
con-comitant MG (Table 27.1).
Tracheal extubation is often predicated on a
tidal vol-ume of 6 mL/kg, negative inspiratory force of –25 cm H2O,
vital capacity of 15 mL/kg, and sustained head-lift for 5 seconds.
Related Topics