Chapter: Clinical Pharmacology: Autonomic nervous system drugs
Cholinergic blocking drugs
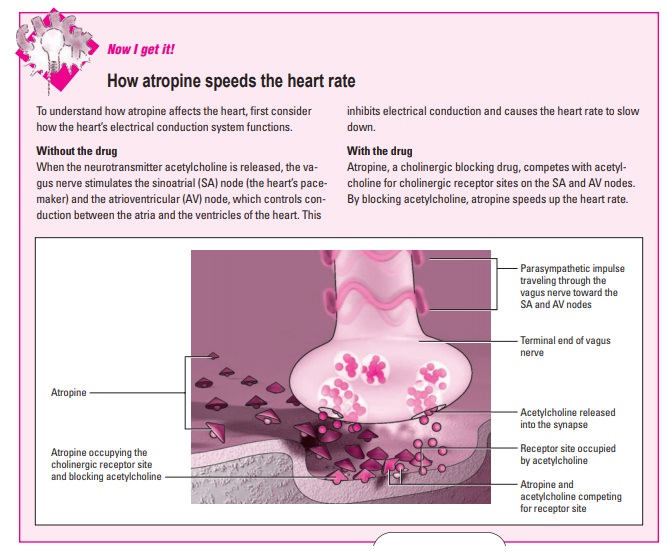
Cholinergic blocking drugs
Cholinergic blocking
drugs interrupt
parasympathetic nerve im-pulses in the central and autonomic nervous systems.
These drugs are also referred to as anticholinergic
drugs because they prevent acetylcholine from stimulating cholinergic
receptors.
Not all receptors are receptive
Cholinergic blocking drugs don’t block all
cholinergic receptors, just the muscarinic receptor sites. Muscarinic receptors
are cholinergic receptors that are stimulated by the alkaloid mus-carine and
blocked by atropine.
First come the belladonna alkaloids
The major cholinergic blocking drugs are the
belladonna alka-loids:
·
atropine (the prototype cholinergic blocking drug)
·
belladonna
·
homatropine
·
hyoscyamine sulfate
·
methscopolamine
·
scopolamine.
Next come their synthetic sisters
Synthetic derivatives of these drugs (the
quaternary ammonium drugs) include:
§ glycopyrrolate
§ propantheline.
And finally the tertiary and quaternary amines
The tertiary amines include:
·
benztropine
·
dicyclomine
·
oxybutynin
·
trihexyphenidyl
·
tolterodine.
Quaternary amines include one drug, trospium.
Atropine may also be used as an antidote for nerve
agents (See the appendix, Vaccines and antidotes for biological and chemical
weapons.)
Let’s talk about it later
Because benztropine and trihexyphenidyl are almost
exclusively treatments for Parkinson’s disease, they’re discussed fully in
chap-ter 3, Neurologic and neuromuscular drugs.
Pharmacokinetics
Here’s how cholinergic blockers move through the
body.
Absorption
The belladonna alkaloids are absorbed from the:
§ eyes
§ GI tract
§ mucous membranes
§ skin.
The quaternary ammonium drugs and tertiary and
quaternary amines are absorbed primarily through the GI tract, although not as
readily as the belladonna alkaloids.
If you want it fast, go I.V.
When administered I.V., cholinergic blockers such
as atropine be-gin to work immediately.
Distribution
The belladonna alkaloids are distributed more
widely throughout the body than the quaternary ammonium derivatives or
dicyclo-mine. The alkaloids readily cross the blood-brain barrier; the other
cholinergic blockers don’t.
Metabolism and excretion
The belladonna alkaloids are only slightly to
moderately protein-bound. This means that a moderate to high amount of the drug
is active and available to produce a therapeutic response. The bel-ladonna
alkaloids are metabolized in the liver and excreted by the kidneys as unchanged
drug and metabolites.
The quaternary ammonium drugs are a bit more complicated. Hydrolysis is
a chemical process whereby a compound cleaved into two or more simpler
compounds occurs in the GI tract and the liver; the drugs are excreted in feces
and urine. Dicyclomine’s metabolism is unknown, but it’s excreted equally in
feces and urine.
Pharmacodynamics
Cholinergic blockers can have paradoxical effects
on the body, de-pending on the dosage and the condition being treated.
Dual duty
Cholinergic blockers can produce a stimulating or
depressing ef-fect, depending on the target organ. In the brain, they do both—
low drug levels stimulate, and high drug levels depress.
Conditional considerations
The effects of a drug on your patient are also
determined by the patient’s disorder. Parkinson’s disease, for example, is character-ized
by low dopamine levels that intensify the stimulating effects of acetylcholine.
Cholinergic blockers depress this effect. In other disorders, however, they
stimulate the central nervous system.
Pharmacotherapeutics
Cholinergic blockers are often used to treat GI
disorders and com-plications.
·
All cholinergic blockers are used to treat spastic or hyperactive
conditions of the GI and urinary tracts because
·
they relax muscles and decrease GI secretions. These drugs may be used
to relax the bladder and to treat urinary incontinence. The quaternary
ammo-nium and amine compounds such as propantheline are the drugs of choice for
these conditions because they cause fewer adverse reactions than belladonna
alkaloids.
·
Belladonna alkaloids are used with morphine to treat biliary col-ic
(pain caused by stones in the bile duct).
·
Cholinergic blocking drugs are given by injection before such diagnostic
procedures as endoscopy and sigmoidoscopy to relax the GI smooth muscle.
Before surgery
Cholinergic blockers such as atropine are given
before surgery to:
·
reduce oral, gastric, and respiratory secretions
·
prevent a drop in heart rate caused by vagal nerve stimulation during
anesthesia.
Brainy belladonna
The belladonna alkaloids can affect the brain. For example,scopolamine,
given with the pain relievers morphine or meperidine, causes drowsiness and
amnesia in a patient having surgery. It’s also used to treat motion sickness.
Belladonna alkaloids also have important
therapeutic effects on the heart. Atropine is the drug of choice to treat:
·
symptomatic sinus bradycardia—when the heart beats too slow-ly, causing
low blood pressure or dizziness (see How
atropinespeeds the heart rate)
·
arrhythmias resulting from the use of anesthetics, choline es-ters, or
succinylcholine.
An eye on the problem
Cholinergic blockers also are used as cycloplegics.
That means that they:
·
paralyze the ciliary muscles of the eye (used for fine focusing)
·
alter the shape of the eye lens.
Moreover, cholinergic blockers act as
mydriatics to dilate the pupils, making it easier to measure refractive errors
during an eye examination or to perform eye surgery.
Punishing pesticides
The belladonna alkaloids, particularly atropine and
hyoscyamine, are effective antidotes to cholinergic and anticholinesterase
drugs. Atropine is the drug of choice to treat poisoning from organophosphate
pesticides. Atropine and hyoscyamine also counteract the effects of the
neuromuscular blocking drugs by competing for the same receptor sites.
Drug interactions
Because cholinergic blockers slow the passage of
food and drugs through the stomach, drugs remain in prolonged contact with the
mucous membranes of the GI tract. This increases the amount of the drug that’s
absorbed and, therefore, increases the risk of ad-verse effects.
Increased effect…
Drugs that increase the effects of cholinergic
blockers include:
§ disopyramide
§ antidyskinetics such as amantadine
§ antiemetics and antivertigo drugs, such as
buclizine, cyclizine, meclizine, and diphenhydramine
§ antipsychotics, such as haloperidol,
phenothiazines, and thio-xanthenes
§ cyclobenzaprine
§ orphenadrine
§ tricyclic and tetracyclic antidepressants.
…or decreased effect
Drugs that decrease the effects of cholinergic
blockers include:
§ cholinergic agonists such as bethanechol
§ anticholinesterase drugs, such as neostigmine
and pyridostig-mine.
Mixing it up some more
Other drug interactions can occur:
·
The risk of digoxin toxicity increases when digoxin is taken with a
cholinergic blocker. Opiate-like
analgesics further slow the movement of food and drugs through the GI tract
when taken with a cholinergic blocker.
·
The absorption of nitroglycerin tablets placed under the tongue is
reduced when this drug is taken with a cholinergic blocker. (See Adverse reactions to cholinergic blockers.)
Related Topics