Chapter: Clinical Pharmacology: Autonomic nervous system drugs
Beta-adrenergic blockers
Adrenergic blocking drugs
Adrenergic blocking drugs, also called sympatholytic drugs, areused to disrupt sympathetic nervous system function. These drugs work by blocking impulse transmission (and thus sympathetic nervous system stimulation) at adrenergic neurons or adrenergic receptor sites. Their action at these sites can be exerted by:
§ interrupting the action of adrenergic (sympathomimetic) drugs
§ reducing available norepinephrine
§ preventing the action of cholinergic drugs.
Classified information
Adrenergic blocking drugs are classified according to their site of action as:
· alpha-adrenergic blockers (or alpha blockers)
· beta-adrenergic blockers (or beta blockers).
Beta-adrenergic blockers
Beta-adrenergic blockers, the most widely used adrenergic block-ers, prevent stimulation of the sympathetic nervous system by in-hibiting the action of catecholamines at beta-adrenergic receptors.
From not so selective…
Beta-adrenergic blockers can be selective or nonselective. Non-selective beta-adrenergic blockers affect:
· beta1 receptor sites (located mainly in the heart)
· beta2 receptor sites (located in the bronchi, blood vessels, and uterus).
Nonselective beta-adrenergic blockers include carteolol, carvedilol, labetalol, levobunolol, metipranolol, penbutolol, pin-dolol, sotalol, nadolol, propranolol, and timolol. (Carvedilol and labetalol also block alpha1 receptors.)
…to highly discriminating
Selective beta-adrenergic blockers primarily affect beta1-adrenergic sites. They include acebutolol, atenolol, betaxolol, bisoprolol, esmolol, and metoprolol.
The not so beta blockers
Some beta-adrenergic blockers, such as pindolol and acebutolol, have intrinsic sympathetic activity. This means that instead of at-taching to beta receptors and blocking them, these beta-adrenergic blockers attach to beta receptors and stimulate them. These drugs are sometimes classified as partial agonists.
Pharmacokinetics
Beta-adrenergic blockers are usually absorbed rapidly and well from the GI tract and are somewhat protein-bound. Food doesn’t inhibit—and may even enhance—their absorption. Some beta-adrenergic blockers are absorbed more completely than others.
Peak by I.V.
The onset of action of beta-adrenergic blockers is primarily dose-and drug-dependent. The time it takes to reach peak concentra-tion levels depends on the administration route. Beta-adrenergic blockers given I.V. reach peak levels much more rapidly than those taken by mouth.
Distribution
Beta-adrenergic blockers are distributed widely in body tissues, with the highest concentrations found in the:
· heart
· liver
· lungs
· saliva.
Metabolism and excretion
Except for nadolol and atenolol, beta-adrenergic blockers are me-tabolized in the liver. They’re excreted primarily in urine, either unchanged or as metabolites, but can also be excreted in feces, bile and, to some degree, breast milk.
Pharmacodynamics
Beta-adrenergic blockers have widespread effects in the body be-cause they produce their blocking action not only at adrenergic nerve endings but also in the adrenal medulla.
A matter of the heart
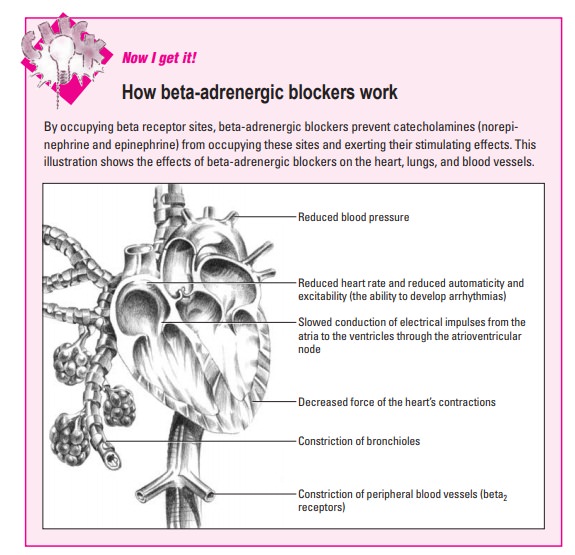
Effects on the heart include increased peripheral vascular resis-tance, decreased blood pressure, decreased force of the heart’s contractions, decreased oxygen consumption by the heart, slowed impulse conduction between the atria and ventricles, and de-creased cardiac output (the amount of blood the heart pumps each minute). (See How beta-adrenergic blockers work.)
Selective and nonselective effects
Some beta-adrenergic blocker effects depend on whether the drug is classified as selective or nonselective.
Selective beta-adrenergic blockers, which prefer to block beta1-receptor sites, reduce stimulation of the heart. They’re often referred to as cardioselective beta-adrenergic blockers.
Nonselective beta-adrenergic blockers, which block both beta1- and beta2-receptor sites, not only reduce stimulation of the heart but also cause the bronchioles of the lungs to constrict. For instance, nonselective beta-adrenergic blockers can cause bron-chospasm in patients with chronic obstructive lung disease. This adverse effect isn’t seen when cardioselective drugs are given at lower doses.
Pharmacotherapeutics
Beta-adrenergic blockers are used to treat many conditions and are under investigation for use in many more. As mentioned previ-ously, their clinical usefulness is based largely (but not exclusive-ly) on how they affect the heart. (SeeAre beta-adrenergic block-ers underused in elderly patients?)
Helping the heart
Beta-adrenergic blockers can be prescribed after a heart attack to prevent another heart attack or to treat:
· angina
· heart failure
· hypertension
· cardiomyopathy (a disease of the heart muscle)
· supraventricular arrhythmias (irregular heartbeats that origi-nate in the atria, SA node, or atrioventricular node).
Jack of all trades
Beta-adrenergic blockers are also used to treat:
· anxiety
· cardiovascular symptoms associated with thyrotoxicosis (over-production of thyroid hormones)
· essential tremor
· migraine headaches
· open-angle glaucoma
· pheochromocytoma (tumor of the adrenal gland).
Drug interactions
Many drugs can interact with beta-adrenergic blockers to cause potentially dangerous effects. Some of the most serious effects in-clude cardiac or respiratory depression, arrhythmias, severe bronchospasm, and severe hypotension that can lead to vascular collapse. Other interactions can also occur:
· Increased effects or toxicity can occur when cimetidine, digox-in, or calcium channel blockers (primarily verapamil) are taken with beta-adrenergic blockers.
· Decreased effects can occur when rifampin, antacids, calcium salts, barbiturates, or anti-inflammatories, such as indomethacin and salicylates, are taken with beta-adrenergic blockers.
· Lidocaine toxicity may occur when lidocaine is taken with beta-adrenergic blockers.
· The requirements for insulin and oral antidiabetic drugs can be altered when these drugs are taken with beta-adrenergic blockers.
· The ability of theophylline to produce bronchodilation is im-paired by nonselective beta-adrenergic blockers.
· Clonidine taken with a nonselective beta-adrenergic blocker can cause life-threatening hypertension during clonidine withdrawal.
· Sympathomimetics taken with nonselective beta-adrenergic blockers can cause hypertension and reflex bradycardia. (See Ad-verse reactions to beta-adrenergic blockers.)
Related Topics