Chapter: Modern Pharmacology with Clinical Applications: Sedative-hypnotic and Anxiolytic Drugs
Benzodiazepines
BENZODIAZEPINES
The benzodiazepines constitute the most commonly used group of
anxiolytics and sedative–hypnotics. Since the
first member of this group, chlordiazepoxide,
was intro-duced, many congeners have been marketed. Most of these drugs possess
anxiolytic, sedative–hypnotic, and anticonvulsant properties. Thus, the
clinical indications for specific benzodiazepines are not absolute. and their
uses overlaps considerably.
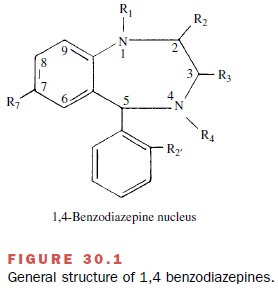
Chemistry
The basic chemical structure
of the benzodiazepines consists of a benzene ring coupled to a seven-member
heterocyclic structure containing two nitrogens (di-azepine) at positions 1 and
4 (Fig. 30.1). Of the 2,000 benzodiazepines that have been synthesized,
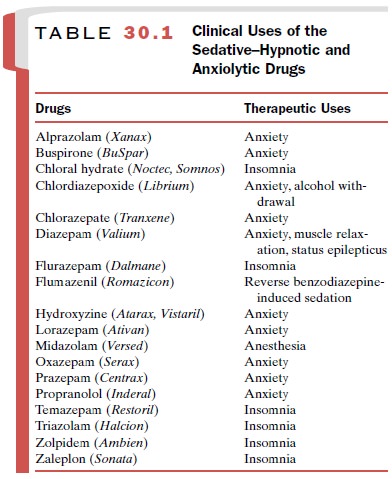
approxi-mately 15 clinically useful compounds are on the mar-ket in the United
States (Table 30.1).
Mechanism of Action
The benzodiazepines bind with high affinity to specific macromolecules within the central nervous system. These benzodiazepine-binding sites (receptors) are closely associated with the receptors for Îł-aminobutyric acid (GABA), which is the major inhibitory neurotrans-mitter in the mammalian brain.
Benzodiazepines poten-tiate GABAergic neurotransmission in
essentially all areas of the central nervous system. This enhancement is
thought to occur indirectly at the postsynaptic GABAA receptor
complex.
The functional significance
of this drug–receptor in-teraction is that the receptor complex regulates the en-trance of chloride into the
postsynaptic cells. The in-crease in chloride conductance mediated by GABA
is intensified by the benzodiazepines. This facilitation of GABA-induced
chloride conductance results in greater hyperpolarization of these cells and
therefore leads to diminished synaptic transmission.
Another chemical class of
sedative–hypnotic drugs, the barbiturates,
also binds to receptors associated with the GABA–chloride ionophore, but these
drugs appear to prolong rather than intensify GABA’s effects. Fig. 24.4 shows
the presumed drug receptor–GABA– chloride ionophore relationship.
In addition to the clinically
useful benzodiazepines, which act as agonists at the benzodiazepine receptor,
at least two other types of ligands also interact with this binding site. These
are the benzodiazepine receptor antagonists
and the inverse agonists. For
example, flumazenil (Romazicon) is a receptor antagonist that
se-lectively blocks the effects of other benzodiazepines at their binding
sites; it has clinical application in the treat- ment of benzodiazepine
overdose and in the reversal of benzodiazepine-induced sedation. The inverse
agonists are compounds that interact with benzodiazepine re-ceptors and
decrease, rather than increase, GABA-mediated changes. They also can antagonize
the effects of benzodiazepine agonists and when administered alone, can be
anxiogenic and proconvulsant.
Pharmacokinetics
Benzodiazepines are usually
given orally and are well absorbed by this route. Since the benzodiazepines are
weak bases, they are less ionized in the relatively alka-line environment of
the small intestine, and therefore, most of their absorption takes place at
this site. For emergency treatment of seizures or when used in anes-thesia, the
benzodiazepines also can be given parenter-ally. Diazepam and lorazepam are
available for intra-venous administration.
The distribution of the
benzodiazepines from blood to tissues and back again is a dynamic process with
con-siderable influence on the onset and duration of the therapeutic effects
produced by these compounds. Those having greater lipid solubility tend to
enter the central nervous system more rapidly and thus tend to produce their
effects more quickly. Several of the ben-zodiazepines have therapeutic effects
that are much shorter in duration than would be predicted based on their rates
of metabolism and excretion; redistribution away from the central nervous
system is of primary im-portance in terminating their therapeutic effects.
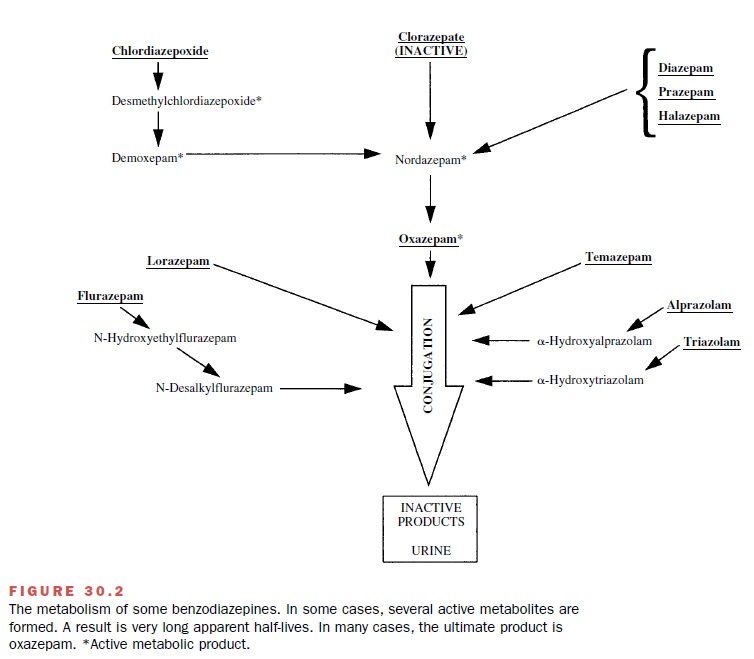
Although tissue
redistribution of benzodiazepines may be an important means of terminating the
actions of selected members of this class of drugs, many benzodi-azepines do
undergo extensive biotransformation. Metabolism takes place both by
dealkylation (phase 1) and conjugation (phase 2) reactions. In many instances,
dealkylation can result in the formation of pharmaco-logically active
compounds. Indeed, most clinically
avail-able benzodiazepines are converted in the liver to one or more active
metabolites. In several cases the active
metabolites have a much longer half-life than the parent compound. In one
case, acid hydrolysis in the stomach converts an inactive compound
(clorazepate) to an ac-tive drug (nordazepam). Figure 30.2 shows the
biotrans-formations involved in the metabolism of representative
benzodiazepines. The water-soluble metabolites of the benzodiazepines are
excreted primarily in the urine.
Since most of the benzodiazepines do undergo bio-transformation, it is possible that changes in liver func-tion may alter the duration of the therapeutic effect produced by these drugs. Despite the fact that few clin-ical studies have demonstrated serious toxicities associ-ated with benzodiazepine administration in individuals with compromised liver function, prudence in the use of these compounds in the elderly and in individuals with liver disease seems advisable.
One of the great
disadvantages associated with many of the sedative and hypnotic drugs (e.g.,
barbitu-rates, propanediol carbamates), which have now largely been replaced by
the benzodiazepines, is the fact that those drugs are very effective inducers
of hepatic drug-metabolizing enzymes. Since the benzodiazepines are only weak
inducers of hepatic microsomal enzymes, they cause relatively few clinically
significant drug in-teractions related to metabolism of other drugs.
Pharmacological Actions
Although it is widely claimed
that the benzodiazepine drugs have a specific calming or anxiolytic effect,
their most prominent and easily quantifiable action is central nervous system
depression. In very low therapeutic doses, this depression manifests as relief
of anxiety that is often accompanied by a feeling of sluggishness or
drowsiness. As the dose is increased, the degree of de-pression is intensified
such that muscle relaxation, hyp- nosis, and a more intense central nervous
system de-pression occur. This depression is related to the ability of these
drugs to facilitate the inhibitory actions of GABA.
A significant advantage of
the benzodiazepines over other central nervous system depressants (e.g., the
bar-biturates) is that they possess a much greater separation between the dose
that produces sleep and the dose that produces death. This increased margin of safety has been one of the major reasons benzodiazepines have largely replaced the
barbiturates and other types of seda-tive–hypnotics in the treatment of anxiety
and insomnia. In addition, benzodiazepine administration is associ-ated
with few side effects.
Clinical Uses
Anxiety
Anxiety disorders are among
the most common forms of psychiatric illness. Anxiety often accompanies other
psychiatric disease and such medical illnesses as angina pectoris,
gastrointestinal disorders, and hypertension.
Anxiety that results from
fear caused by an acute illness or a stressful event, such as a divorce or the
loss of a loved one, is usually self-limiting and can be of rela-tively short
duration. Other disorders that have anxiety as a component are not necessarily
associated with a life event, and may persist for considerable periods, even
throughout the individual’s life.
Both acute and chronic anxiety can be treated with benzodiazepines,
although
it is anticipated that for most anxiety
disorders counseling will also play an important role. Benzodiazepines employed
in the treatment of anxiety should be used in the lowest effective dose for the
shortest duration so that they will provide maxi-mum benefit to the patient
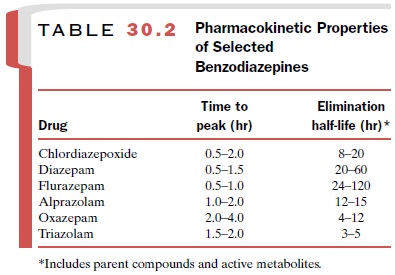
while minimizing the poten-tial for adverse reactions. For most types of anxiety,
none of the benzodiazepines is therapeutically superior to any other. Choice of
a particular agent is usually made on the basis of pharmacokinetic (Table 30.2)
con-siderations. A benzodiazepine with a long half-life should be considered if
the anxiety is intense and sus-tained. A drug with a short half-life may have
advan-tages when the anxiety is provoked by clearly defined circumstances and
is likely to be of short duration.
Insomnia
All of the benzodiazepines will produce sedative– hypnotic effects
of sufficient magnitude to induce sleep, provided that the dose is high enough.
However,
the aim in the treatment of sleep
disorders is to induce sleep that is as close as possible to natural sleep so
that the patient falls asleep quickly, sleeps through the night, and has sleep
of sufficient quality to awake refreshed.
Extensive sleep studies have been conducted with a variety of sedative–hypnotic drugs, and all of these drugs appear to alter the normal distribution of rapid eye movement (REM) and non-REM sleep. Most of the older sedative–hypnotic agents markedly depress REM sleep. In contrast, when the benzodiazepines are used in appropriate doses, they depress REM sleep to a much smaller extent.
As with treatment of anxiety, the choice of a particular
benzodiazepine to treat a sleep distur-bance is again generally based on
pharmacokinetic cri-teria. While longer-acting compounds may ensure that a
patient will sleep through the night, they also may cause cumulative effects
resulting in daytime sluggishness or drug hangover. Shorter-acting compounds
avoid the hangover problem, but their use may be associated with early
awakening and an increase in daytime anxiety.
Epilepsy and Seizures
Nearly all central nervous
system depressants have some capacity to suppress seizures by virtue of their
de-pressant activity on the brain and spinal cord. Clonazepam and diazepam are
two benzodiazepines that depress epileptiform activity and are used in the
treatment of epilepsy and seizure disorders .
Sedation, Amnesia, and Anesthesia
Benzodiazepines have the
capacity to produce a calm-ing effect and to cause anterograde amnesia, in which the patient cannot recall events that
took place for some time after the drug was administered.
Benzo-diazepine-induced sedation and amnesia are deemed useful in the
preparation of patients for anesthesia, surgery, and other frightening or
unpleasant medical and dental procedures and diagnostic tests. Midazolam is a
frequently used anesthetic benzodiazepine .
Muscle Relaxation
Benzodiazepines have the
capacity to depress polysyn-aptic reflexes and have been shown to decrease
decere-brate rigidity in cats and spasticity in patients with cere-bral palsy.
What is not clear is whether they can, in humans, relax voluntary muscles in
doses that do not cause considerable central nervous system depression.
Nevertheless, benzodiazepines, such as diazepam, are often prescribed for
patients who have muscle spasms and pain as a result of injury. In these
circumstances, the sedative and anxiolytic properties of the drug also may
promote relaxation and relieve tension associated with the condition.
Alcohol and Sedative–Hypnotic Withdrawal
Withdrawal from long-term
high-dose use of alcohol or sedative–hypnotic drugs can be life threatening if
phys-ical dependence is present. Benzodiazepines, such as chlordiazepoxide (Librium) and diazepam (Valium), are sometimes used to lessen
the intensity of the with-drawal symptoms when alcohol or sedative–hypnotic
drug use is discontinued. Benzodiazepines are also em-ployed to help relieve
the anxiety and other behavioral symptoms that may occur during rehabilitation.
Adverse Effects and Toxicities
Most adverse effects
associated with use of the benzodi-azepines are related to their ability to
produce central nervous system depression. These include drowsiness, ex-cessive
sedation, impaired motor coordination, confusion, and memory loss.These effects
are most troublesome dur-ing the initial week or two of treatment.
Subsequently, the patient becomes tolerant and these effects produce less
difficulty. Although for most individuals these symptoms are mild, patients
should be cautioned against engaging in potentially dangerous tasks such as
operating machinery or driving a car during the initial treatment period.
Less common adverse effects
include blurred vision, hallucinations, and paradoxical reactions consisting of
excitement, stimulation, and hyperactivity. Also, a vari-ety of
gastrointestinal complaints occur, and blood dyscrasias have been reported, but
these are rare. Benzodiazepine administration during pregnancy, deliv-ery, or
lactation has the potential to have adverse effects on the fetus or newborn.
As with other central nervous
system depressants, the effects of benzodiazepines are additive with those of
ethanol. Patients should be warned that ethanol-containing
beverages may produce a more profound de-pression when taken simultaneously
with a benzodi-azepine.
One of the major reasons for
the popularity of the benzodiazepines is their relative safety. Overdoses with
the benzodiazepines occur commonly, but fatal toxic oc-currences are rare.
Fatal intoxications are more likely in children, in individuals with
respiratory difficulties, and in individuals who have consumed another central
ner-vous system depressant, such as alcohol. After an over-dose, the patient
begins a deep sleep that may last for 24 to 48 hours, depending on the dose.
However, even with large overdoses, the patient can usually still be aroused.
Tolerance and dependence do occur with the use of benzodiazepines. Discontinuation of drug
administra-tion, particularly abrupt withdrawal, can be associated with a
variety of symptoms, including rebound insomnia and rebound anxiety. The level
of insomnia or anxiety may even exceed that which preceded the treatment.
Usually, a gradual tapering of the dose
until it is eventu-ally discontinued lessens the likelihood of a withdrawal
reaction, although in some individuals even this method of drug removal can result in anxiety, apprehension, tension,
insomnia, and loss of appetite. More severe symptoms may occur when an
individual withdraws from a supratherapeutic dose, particularly if the drug has
been taken for months or years. These symptoms can include, in addition to
those already mentioned, muscle weakness, tremor, hyperalgesia, nausea,
vomit-ing, weight loss, and possibly convulsions.
Drug Interactions
When used with other
sedative–hypnotics or alcohol, the benzodiazepines will produce additive
central ner-vous system depression.
Many benzodiazepines are
metabolized by the cy-tochrome P450 (CYP) enzyme designated CYP3A4. CYP3A4 is
inhibited by grapefruit juice and by drugs such as ketoconazole, itraconazole,
nefazodone, eryth-romycin, and ritonavir. Coadministration of these sub-stances
along with a benzodiazepine may result in in-tensification and prolongation of
the benzodiazepine effect. Conversely, rifampin, carbamazepine, and phe-nytoin
can induce the CYP3A4 enzyme, and therefore their coadministration can reduce
the therapeutic effect of the benzodiazepines.
Related Topics