Chapter: Essentials of Psychiatry: Anxiolytic Drugs
Anxiolytic Drugs
Anxiolytic Drugs
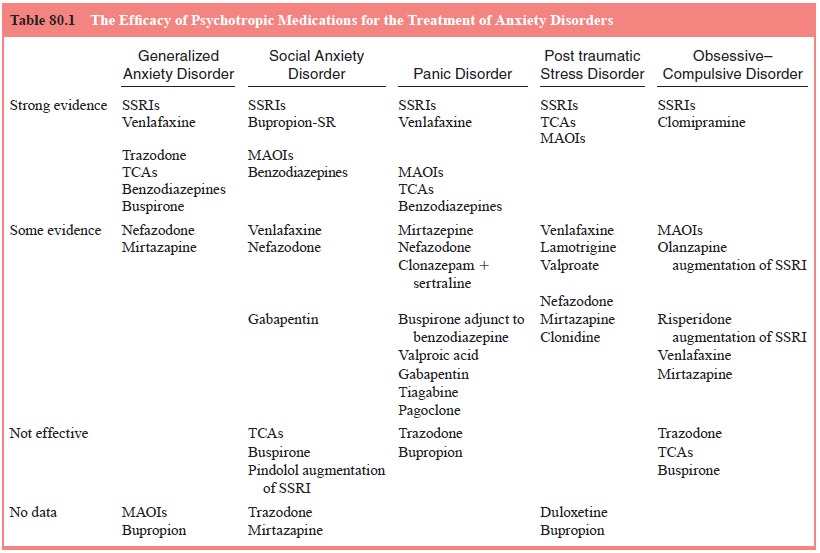
In the
last decade, there has been a substantial increase in the number of medications
demonstrated to be effective for the treat-ment of anxiety and anxiety
disorders (Table 80.1).
There was
a cascade of anxiolytic research in the 1990s. The selective serotonin reuptake
inhibitors (SSRIs) as a class were demonstrated to be efficacious treatments
for most of the anxiety disorders described in the DSM-IV-TR. Although these
agents have a delayed onset when contrasted with the benzodiazepines, they have
a broader spectrum of action, no problems with depen-dence, and much less of a
problem with withdrawal syndromes. The 1990s also saw the approval of
venlafaxine as a treatment for generalized anxiety disorder.
A General Approach to Using Medication with Anxious Patients
Making an
appropriate differential diagnosis which includes a DSMIV-TR anxiety disorder
is critical to the success of any psychopharmacological intervention. The
diagnosis dictates the class of medication to be used and the length of
pharmacother-apy. An important rule in general is “to start low and go slow”
when initiating pharmacological treatment for patients with anxiety disorders.
Interestingly, although treating patients with anxiety disorders frequently
requires a more gradual initial titra-tion schedule, patients frequently attain
maintenance dosages of antidepressant medications that are greater than the
dosage com-monly used to treat major depressive disorder.
Antidepressant Medication
It has
been known that medications initially identified because of their antidepressant
properties are frequently effective treat-ments for anxiety disorders as well.
The basic action of the majority of the antidepressants is to increase the
availability of neurotransmitters in the synaptic cleft. These agents have the
broadest spectrum of activity which spans the entire spectrum of DSM-IV-TR
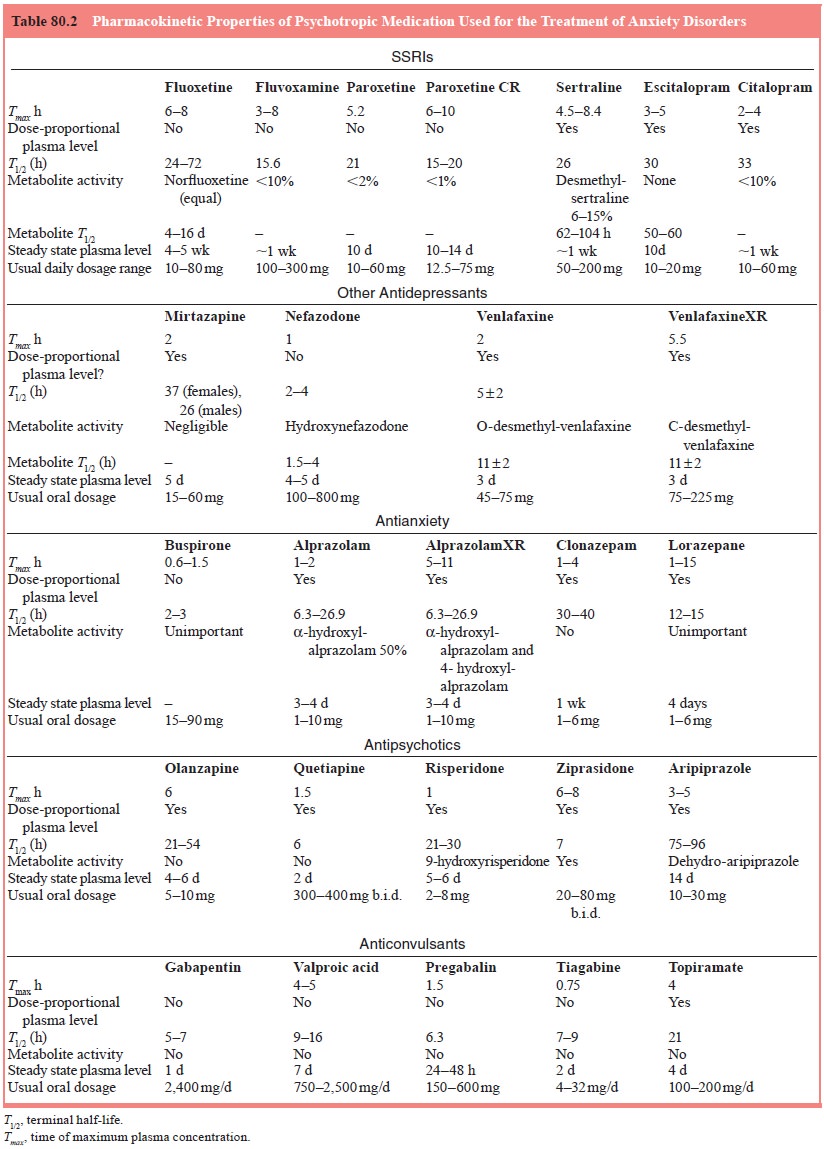
anxiety disorders. The relative differences in terms of major pharmacokinetic
and pharmacodynamic properties are outlined in Tables 80.2 and 80.4. As
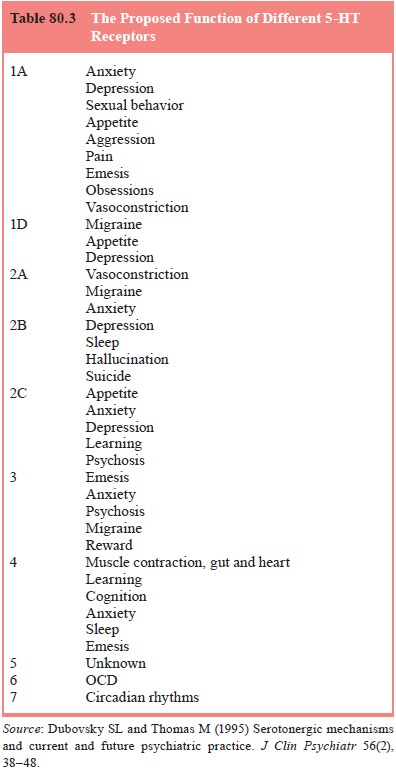
illustrated in Table 80.1, a variety of serotonin receptor subtypes have been
implicated in the modulation of anxiety disorders, depressive disorders,
mi-graine, pain and neuropsychiatric disorders.

Indications for Selective Serotonin Reuptake Inhibitors
Initial
data from randomized, placebo-controlled treatment trials suggest that SSRIs
may be useful in the treatment of adults and children with generalized anxiety
disorder. SSRIs have emerged as a first-line treatment for social anxiety
disorder. Most of the efficacy data are derived from multicenter, double-blind
trials of paroxetine, sertraline and fluvoxamine.
In
addition, SSRIs are generally accepted as a first-line treat-ment for panic
disorder. The major advantage of these agents is their tolerability and thus
longer-term acceptance by patients. There is evidence that fluoxetine,
sertraline, paroxetine, fluvoxamine and citalopram are effective in the acute
treatment of panic disorder.
One of
the advantages of SSRIs is that they tend to be fairly well tolerated in
contrast to some of the other treatments available for panic disorder. Although
a few individuals may have some initial problems with restlessness and
increased anxiety, data suggest that starting at lower doses such as 25 mg/day
of sertraline or 10 mg/day of paroxetine may decrease the risk of
antidepressant “jitteriness”.
There
have been open-label and double-blind, placebo-controlled studies demonstrating
that SSRIs are effective for the treatment of post traumatic stress disorder
(PTSD). Open-label trials with all of the SSRIs currently available suggest
that each may be effective in decreasing the core symptoms of PTSD.
Large,
well-designed, double-blind, placebo-controlled trials demonstrate that
fluoxetine, paroxetine, fluvoxamine, cital-opram and sertraline are effective
acute treatments for obses-sive–compulsive disorders.
Indications for Serotonin–Norepinephrine Reuptake Inhibitors in Anxiety Disorders
Venlafaxine
There
have been a number of placebo-controlled multicentered studies demonstrating
that venlafaxine XR is an effective treat-ment of GAD.
Doses as
low as 37.5 mg/day and as high as 225 mg/day are effective in decreasing
symptoms of anxiety for patients with GAD. Side effects appear to be mild and
tend to decrease in num-ber and intensity over the course of treatment. Nausea,
dry mouth and somnolence are the most commonly repeated side effects.
Case
reports and open-label studies have been published for use of venlafaxine in
social anxiety disorder (Kelsey, 1995).
There is
only one double-blind, placebo-controlled study by Pollack and coworkers.
(1996) suggesting that venlafaxine may be an effective treatment for patients
with panic disorder.
Indications for Tricyclic Antidepressant Medication and Monoamine Oxidase Inhibitors in Anxiety Disorders
A variety of tricyclic antidepressants (TCAs) have been dem-onstrated to be effective treatments for GAD. However, the side effects and difficulty titrating the dosage of these medications have made their use uncommon.
In
general, TCAs have not been found to be effective for the treatment of social
anxiety disorder, but there is evidence of effectiveness in panic disorder.
Although surpassed by the SSRIs as first-line agents, there is no doubt that
first-generation MAOIs are effective. Unfortunately, the risk of hypertensive
crisis and the need for patients to follow a tyramine-free diet makes this
class of drugs unappealing for the majority of patients.
Although
TCAs have been widely used for the treatment of panic disorder, their
side-effect profile and slow time to onset of action makes them a difficult
class of medication for many patients to tolerate.
There
have been seven meta-analyses comparing and con-trasting clomipramine and SSRIs
(Abramowitz, 1997; Cox et al., 1993;
Greist, 1998; Kobak et al., 1998;
Piccinelli et al., 1995; Stein et al., 1995). In each case,
clomipramine has been found to be significantly more effective than the SSRIs.
If one takes the entire body of evidence as a whole into account, analyses sug-gest
that clomipramine is at least as effective as the SSRIs and may, in some
instances, be more effective (Greist, 1998; Todorov et al., 2000).
Other Antidepressant Medication (Bupropion, Mirtazapine, Nefazodone, Trazodone) in Anxiety Disorders
Most evidence
fails to support these medications as a first-line treatment for generalized
anxiety disorders, social anxiety disor-der, panic disorder, PTSD, or
obsessive-compulsive disorder.
Benzodiazepine Medication
The
benzodiazepines as a class work by increasing the relative efficiency of the
gamma-aminobutyric acid (GABA) receptor when stimulated by GABA. The
benzodiazepines bind to a site located adjacent to the GABA receptor and cause
an allosteric change to the receptor that facilitates the increased passage of
the chloride ions intracellularly when GABA interacts with the receptor
complex. This leads to a relative hyperpolarization of the neuronal membrane
and inhibition of activity in the brain. The benzodiazepines as a group have
different affinities for GABA receptors, in fact some agents bind to only one
of the two types of GABA receptors. The relative pharmacodynamic and
pharmacokinetic properties of the benzodiazepines are fur-ther outlined in
comparison to the other medications in Table 80.2. As a class, benzodiazepines
are efficacious for the treat-ment of panic disorder, social anxiety disorder,
generalized anxiety disorder, alcohol withdrawal and situational anxiety. The
choice of an agent should take into account the age, medical health and comorbid
diagnosis of the patient. Although obses-sive–compulsive disorder falls within
the taxonomy of anxiety disorders, benzodiazepines do not seem to be
particularly effec-tive in treating these patients.
The
limitations to these drugs are the same as when used in any indication. Due to
the potential for abuse and drug with-drawal, their use must be monitored
carefully. This is a particu-larly problematic issue in social anxiety disorder
because of the high rate of comorbid substance abuse. Benzodiazepines may be
best suited for patients with situational and performance anxiety on an
as-needed basis.
The two
high potency benzodiazepines that have been approved by the FDA, alprazolam and
clonazepam are widely used in the treatment of panic disorder. They may also be
help-ful as adjuncts in the treatment of obsessive-compulsive disorder, though
not as first-line stand alone treatments.
Buspirone
Buspirone
is a member of the group of agents called azaspi-rodecanediones. It is believed
to exert its anxiolytic effect by acting as a partial agonist at the 5-HT1A
autoreceptor. Stimu-lation of the 5-HT1A autoreceptor causes
decrease release of serotonin into the synaptic cleft. However, buspirone also
exerts another effect through its active metabolite 1-phenyl-piperazine (1-PP)
that acts on alpha-2-adrenergic receptors to increase the firing rate of the locus
coeruleus. Some not yet well-characterized
combination of these effects may be responsible for anxiolytic effect of
buspirone. It usually takes approximately 4 weeks for the benefit of buspirone
therapy to be noticed in patients with GAD. It may also be a useful adjuvant in
some patients with treatment resistant panic disor-der. One major advantage of
buspirone is that it does not cross react with benzodiazepines. The most common
side effects associated with buspirone include dizziness, gastrointestinal
distress, headache, numbness and tingling. The most common pharmacokinetic and
pharmacodynamic actions of buspirone are described in Table 80.3.
Beta-blocker Medication
Beta-adrenergic
blockers competitively antagonize norepi-nephrine and epinephrine at the
beta-adrenergic receptor. It is thought that the majority of positive effects
of beta-blockers are due to their peripheral actions. Beta-blockers can
decrease many of the peripheral manifestations of anxiety such as tachy-cardia,
diaphoresis, trembling and blushing. The advent of more selective beta-blockers
that only block the beta-2-adren-ergic receptor has been beneficial since
blockade of beta-1 ad-renergic receptors can be associated with bronchospasm.
Beta-blockers may be useful for individuals who have situational anxiety or
performance anxiety. They generally have not been effective in treating anxiety
disorders such as generalized so-cial anxiety disorder, panic disorder, or
obsessive–compulsive disorder.
Anticonvulsant Medication
One of
the areas of increasing research is the study of an-ticonvulsants in anxiety
disorders. Currently, there are few published placebo-controlled studies
investigating the effi-cacy of commonly used anticonvulsants for the treatment
of anxiety or anxiety disorders. There is one published report of a large
double-blind, placebo-controlled study of gabap-entin for the treatment of
social anxiety disorder. The precise mechanism of action of gabapentin is not
fully appreciated, however, it is thought gabapentin somehow increases brain
GABA levels.
Antipsychotic Medication
The conventional or typical antipsychotic medication whose mechanism of action is primarily to block dopamine Type-2 re-ceptors has been used as adjuvant medication for the treatment of anxiety disorders for years. However, because of problems with extrapyramidal side effects and the risk of developing tardive dyskinesia, these agents had fallen out of favor. The newer class of atypical antipsychotic medications have a decreased risk of both extrapyramidal side effects and tardive dyskinesia and so antipsychotic medications are beginning to be used again as adju-vants in patients with treatment resistant anxiety disorders. This simultaneous blockade of both neurotransmitter systems seems to decrease extrapyramidal side effects and the risk of develop-ing tardive dyskinesia. Although the different atypical antipsy-chotic medications have different affinities for dopamine Type-2 and serotonin Type-2 receptors, this is the common mechanism of action of these agents. The atypical antipsychotic medica-tions also differ dramatically in terms of their pharmacodynamic properties. There are very few published studies investigating atypical antipsychotic medication augmentation for the treatment of anxiety disorders, so it is not possible to recommend their use as a first-line treatment for anxiety disorders.
Related Topics