Chapter: Medicine Study Notes : Health Care of the Elderly
Ageing - Health Care of the Elderly
Ageing
·
Net effect of age related of
age related changes ® likelihood of dying
·
Age related changes affect all
body systems: cardiac, respiratory, CNS, musculoskeletal, vision, hearing,
skin, immune and renal
·
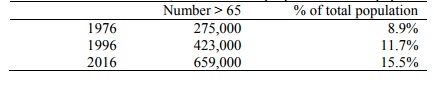
Demographics:
·
In
absolute number of 60, and > 60s as a proportion of total population
Concepts
·
Cohort Effect: Each current age
group (eg adults now aged 80 – 90) have experienced a distinctive history,
leading to the following cohort effects:
o Disease and disability with roots in environmental exposure varies from
cohort to cohort (eg tobacco use, diet, peak bone mass)
o Cross sectional studies should consider cohort effect (eg medical care available
to 80 year olds when they were 30, compared with 30 year olds now). A
difference may not be due solely to aging
o Cultural and social differences between cohorts: eg response to health
professionals, access to services, gender and spiritual issues
·
Diversity of physiology and
function increases with age: stereotypes are unhelpful, need individual
assessment
·
Multiple pathology: Not a single
disease process presenting acutely, but a person presenting with disease(s)
and/or disabilities. Need a model of care and assessment that considers
individual disease processes, individual experience, the social context, and
interactions between and within these dimensions
·
Failure to present (professionals
need to initiate strategies to overcome):
o Self stereotyping: I‟m just old, there‟s nothing they can do, etc
o Cognitive impairment and depression
o Disability: eg ¯mobility
·
Atypical presentation: Strange or
unusual presentations are more common compared with younger people, due to
multiple diseases, reduced homeostatic capability, etc. Can be non-specific
(not coping, immobile, etc)
·
Threshold effect: Change in
functional status can occur in the absence of a clear precipitant due to build
up of subclinical dysfunction and loss of physiologic reserve
·
Disordered homeostasis and the
cascade effect: Age related effects ® ¯ability to maintain homeostasis
in the presence of a threat (eg medication). Disordered homeostasis in one
system can trigger dysfunction in another
·
Caring for carers is important in
maintaining people in the environment of their choice
Disability
·
Disability is understood by (WHO
definition):
o Pathology: abnormal structure or function of an organ or system. Eg osteoarthritis
o Impairment: Loss or abnormality of psychological, anatomical or physiological function. In decreasing order of prevalence in the elderly these are (in a CHCH study): visual impairment, hypertension, symptomatic spinal osteoporosis, hearing impairment, stroke/TIA, osteoarthritis of the hip or knee, urinary incontinence, dementia, postural hypotension
o Disability: Any restriction or lack of ability to perform a task or activity. Eg for elderly women in
o Mosgiel: housekeeping, shopping, bathing, mobility
o Handicap: disadvantage for a particular individual resulting from impairment or disability that limits fulfilment of a role normal for someone of that age, culture, gender, etc. Eg reading a newspaper, shopping, etc
o However, some things don‟t fit well into this model (eg psychiatric illness). WHO currently revising. Will also include impact of environment (eg not being able to drive is not always a disability – eg if you live in the 3rd world)
·
Interventions should address all
levels, and acknowledge the interaction between each level
·
Reported disability has a clear
age associated increase
Related Topics