Chapter: Pathology: Inflammation
Acute Inflammation
ACUTE INFLAMMATION
Acute
inflammation is an immediate response to injury or infection, which is part of
innate immunity.
·
Short duration in normal host
·
Cardinal signs of inflammation
include rubor (redness); calor (heat); tumor (swelling); dolor (pain); functio
laesa (loss of function).
The
important components of acute inflammation are hemodynamic changes, neu-trophils, and chemical mediators.
Hemodynamic Changes
1)
Initial transient vasoconstriction
2)
Massive vasodilatation mediated by
histamine, bradykinin, and prostaglandins
3)
Increased vascular permeability
·
Chemical mediators of increased
permeability include vasoactive amines (histamine and serotonin), bradykinin
(an end-product of the kinin cas-cade), leukotrienes (e.g., LTC4, LTD4, LTE4).
·
The mechanism of increased vascular
permeability involves endothelial cell and pericyte contraction; direct
endothelial cell injury; and leuko-cyte injury of endothelium.
4)
Blood flow slows (stasis) due to
increased viscosity, allows neutrophils to marginate
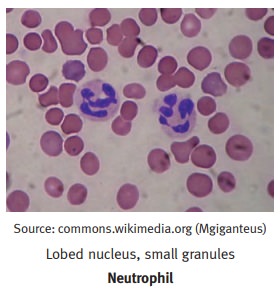
Neutrophils
·
Life span in tissue 1–2 days
·
Synonyms: segmented neutrophils,
polymorphonuclear leukocytes (PMN)
·
Primary (azurophilic) granules
contain myeloperoxidase, phospholipase A2, lysozyme (damages bacterial cell
walls by catalyzing hydrolysis of 1,4-beta-linkages), and acid hydrolases. Also
present are elastase, defensins (microbicidal peptides active against many
gram-negative and gram-positive bacteria, fungi, and enveloped viruses), and
bactericidal permeability increasing protein (BPI).
·
Secondary (specific) granules
contain phospholipase A2, lysozyme, leukocyte alkaline phosphatase (LAP),
collagenase, lactoferrin (chelates iron), and vita-min B12-binding proteins.
·
Macrophages
(life span in tissue compartment is 60–120 days) have
acidhydrolases, elastase, and collagenase.
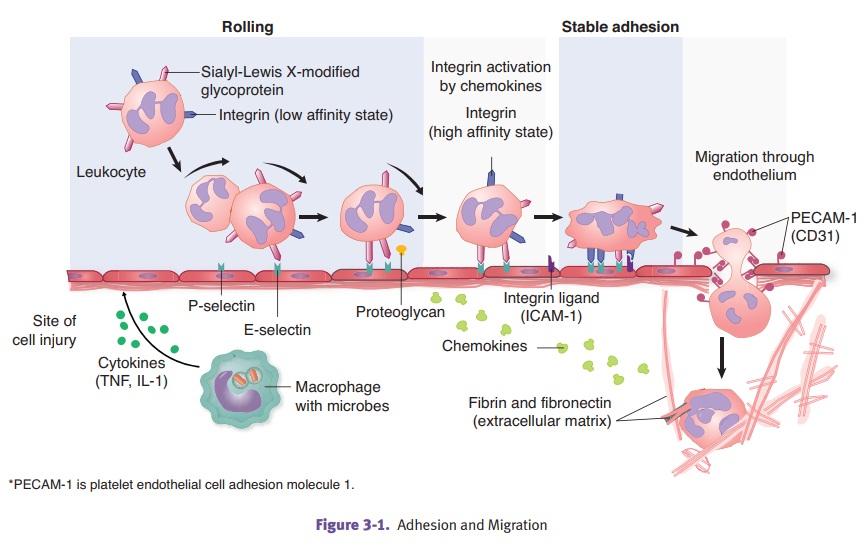
Neutrophil margination and adhesion.Adhesion
is mediated by complementarymolecules on the surface of neutrophils and
endothelium.
·
In step 1, the endothelial cells at sites of inflammation have
increased expres-sion of E-selectin
and P-selectin.
·
In step 2, neutrophils weakly bind to the endothelial selectins and
roll along the surface.
·
In step 3, neutrophils are stimulated by chemokines to express their
integrins.
·
In step 4, binding of the integrins to cellular adhesion molecules
(ICAM-1 and VCAM-1) allows the neutrophils to firmly adhere to the endothelial
cell.
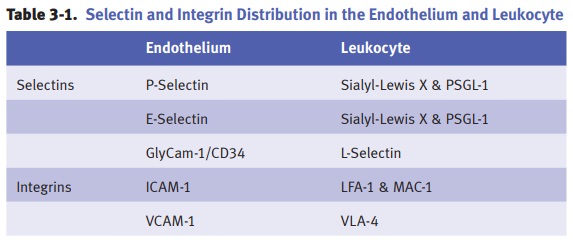
Modulation of adhesion molecules in
inflammation occurs as follows. The fast-est step involves redistribution of
adhesion molecules to the surface; for example, P-selectin is normally present
in the Weibel-Palade bodies of endothelial cells and can be mobilized to the
cell surface by exposure to inflammatory mediators such as histamine and
thrombin.
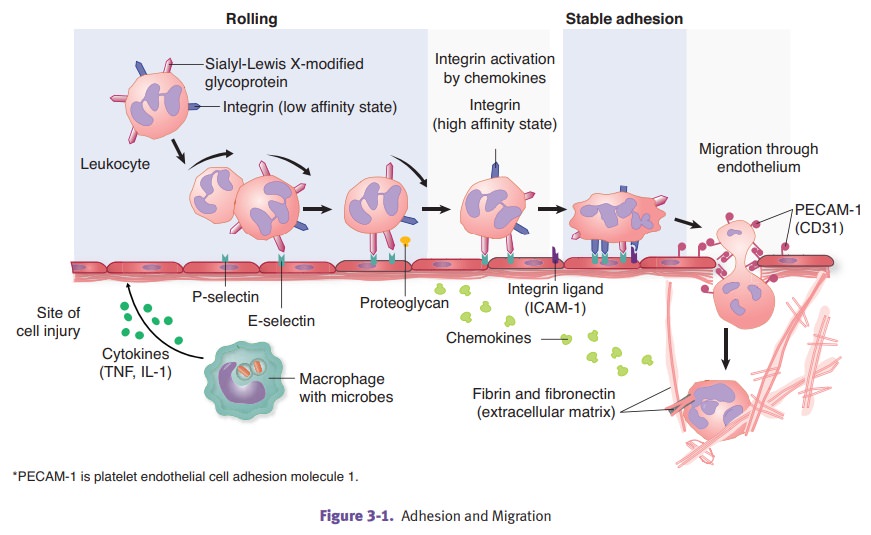
·
Additionally, synthesis of adhesion
molecules occurs. For example, proinflam-matory cytokines IL-1 and TNF induce
production of E-selectin, ICAM-1, and VCAM-1 in endothelial cells.
·
There can also be increased binding
affinity, as when chemotactic agents cause a conformational change in the
leukocyte integrin LFA-1, which is converted to a high-affinity binding state.
Defects
in adhesion can be seen in diabetes mellitus, corticosteroid use, acute alcohol
intoxication, and leukocyte adhesion deficiency (autosomal recessive condition
with recurrent bacterial infections).
In
emigration (diapedesis), leukocytes
emigrate from the vasculature (postcapil-lary venule) by extending pseudopods
between the endothelial cells. They then move between the endothelial cells,
migrating through the basement membrane toward the inflammatory stimulus.
Chemotaxis is
the attraction of cells toward a chemical mediator that is releasedin the area
of inflammation. Important chemotactic factors for neutrophils include
bacterial products such as N-formyl-methionine
and host derived molecules such as leukotriene B4 (LTB4), complement system
product C5a, and α-chemokines
(IL-8).
Phagocytosis and degranulation.Opsonins
coat microbes to enhance their detec-tion and phagocytosis. Important opsonins
include the Fc portion of IgG isotypes, complement system product C3b, and
plasma proteins such as collectins (which bind to bacterial cell walls).
Engulfment
occurs when the neutrophil sends out cytoplasmic processes that sur-round the
bacteria. The bacteria are then internalized within a phagosome. The phagosome
fuses with lysosomes (degranulation).
Defects
in phagocytosis and degranulation include Chédiak-Higashi syndrome, an
autosomal recessive condition characterized by neutropenia. The neutrophils
have giant granules (lysosomes) and there is a defect in chemotaxis and
degranulation.
Intracellular killing.
In oxygen-dependent killing, respiratory
burst requires oxygen and NADPHoxidase and produces superoxide, hydroxyl
radicals, and hydrogen peroxide. Myeloperoxidase requires hydrogen peroxide and
halide (Cl–) and produces HOCl (hypochlorous
acid).
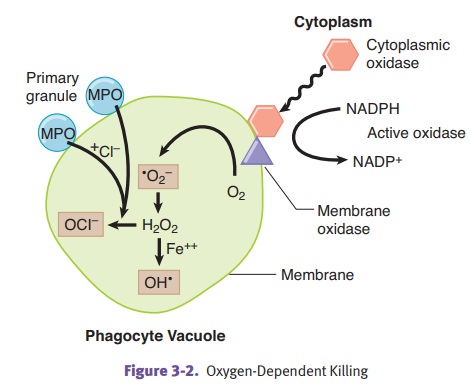
Oxygen-independent killing involves
lysozyme, lactoferrin, acid hydrolases, bac-tericidal permeability increasing
protein (BPI), and defensins.
Deficiencies
of oxygen-dependent killing include:
·
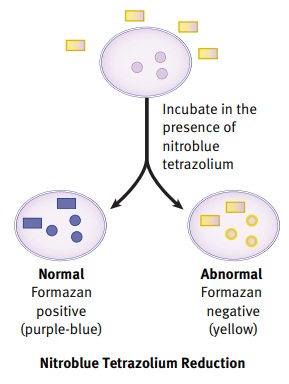
Chronic granulomatous disease of childhood
can be X-linked or autosomal recessive. It is characterized by a deficiency of
NADPH oxidase, lack of super-oxide and hydrogen peroxide, and recurrent
bacterial infections with catalase-positive organisms (S. aureus). The nitroblue tetrazolium test will be negative.
·
Myeloperoxidase deficiency is an
autosomal recessive condition characterized by infections with Candida. In contrast to chronic
granulomatous disease, the nitroblue tetrazolium test will be positive.
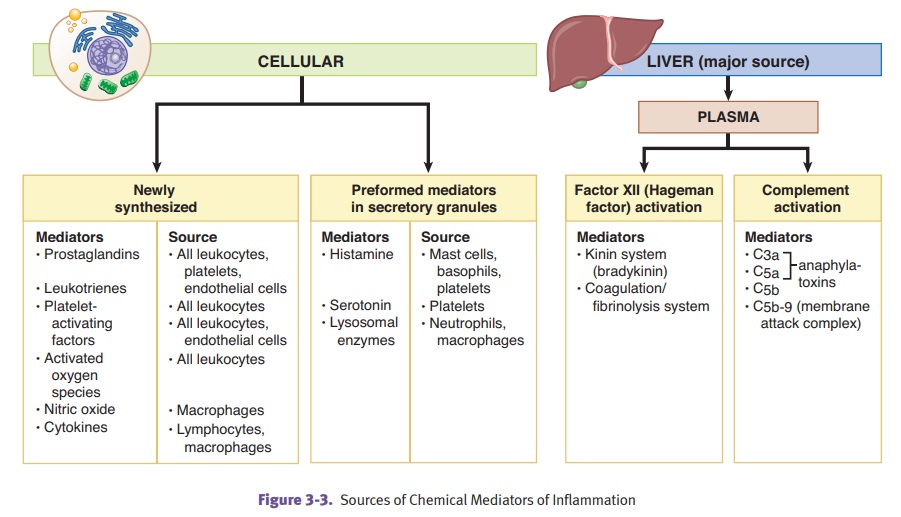
Chemical Mediators of Inflammation
Vasoactive amines
·
Histamine
is produced by basophils, platelets, and mast cells. It
causes vaso-dilation and increased vascular permeability. Triggers for release
include IgE-mediated mast cell reactions, physical injury, anaphylatoxins (C3a
and C5a), and cytokines (IL-1).
·
Serotonin
is produced by platelets and causes vasodilation and
increased vas-cular permeability.
Kinin system
·
Activated Hageman factor (factor
XII) converts prekallikrein →
kallikrein
·
Kallikrein cleaves high molecular
weight kininogen (HMWK) →
bradykinin
·
Effects of bradykinin include
increased vascular permeability, pain, vasodila-tion, bronchoconstriction, and
pain
Arachidonic acid products
Cyclooxygenase pathway
·
Thromboxane A2 is produced by platelets and causes
vasoconstriction and platelet aggregation.
·
Prostacyclin (PGI2) is produced by vascular endothelium and
causes vasodilation and inhibition of platelet aggregation.
·
Prostaglandin E2 causes pain.
·
Prostaglandins PGE2, PGD2, and PGF2 cause vasodilatation.
Arachidonic acid products
Lipoxygenase pathway
Leukotriene
B4 (LTB4) causes neutrophil chemotaxis, while leukotriene C4, D4, E4 cause
vasoconstriction. Lipoxins are antiinflammatory products which inhibit
neutrophil chemotaxis.
Important products in the complement
cascade include C5b-C9 (membrane attackcomplex), C3a,C5a (anaphylatoxins
stimulate the release of histamine), C5a (leuko-cyte chemotactic factor), and
C3b (opsonin for phagocytosis).
Cytokines
·
IL-1 and TNF cause fever and induce
acute phase reactants; enhance adhe-sion molecules; and stimulate and activate
fibroblasts, endothelial cells, and neutrophils.
·
IL-8 is a neutrophil chemoattractant
produced by macrophages.
Four Outcomes of Acute Inflammation
·
Complete resolution with
regeneration
·
Complete resolution with scarring
·
Abscess formation
·
Transition to chronic inflammation