Chapter: Essentials of Psychiatry: Mood Disorders: Bipolar (Manic–Depressive) Disorders
A “Bipolar” Disorder?
A “Bipolar” Disorder?
Classically, mania has been considered to be the opposite of
de-pression: manic individuals were said to be cheery, optimistic and
self-confident, hence the name bipolar disorder. However, in most descriptive
studies, substantial proportions of hypomanic and manic patients actually
exhibit substantial dysphoric symp-toms. Mixed episodes, defined as the
simultaneous occurrence of full-blown manic and depressive episodes, are the
most promi-nent example of dysphoria during mania.
Additional Features: Psychosis and Rapid Cycling
Psychosis can occur in either pole of the disorder. If psychotic symptoms are limited to the major mood episode, the individual is considered to have manic–depressive disorder with psychotic features. On the other hand, if psychotic symptoms endure signif-icantly into periods of normal mood, the diagnosis of schizoaffec-tive disorder is made. For formal research diagnostic criteria and DSM definitions, 2 weeks of psychotic symptoms during normal mood is sufficient to convert a diagnosis of manic–depressive or major depressive disorder into schizoaffective disorder, because it is thought that such persons have a clinical course midway between individuals with mood disorders or schizophrenia. However, this cutoff point is fairly arbitrary, and its validity is not well established. For example, it may be that psychotic symptoms actually represent a separate, comorbid disorder, or they may be integral features of severe manic–depressive disorder that simply take longer to resolve. Identification of pathophysiological and genetic bases of psychosis and of manic–depressive disorder will certainly help to resolve these issues.
Rapid cycling is defined by the occurrence of four or more mood episodes
within 12 months. It should be noted that, despite the name, the episodes are
not necessarily or even commonly truly cyclical; the diagnosis is based simply
on episode counting. This subcategory is of significance because it predicts a
relatively poorer outcome and worse response to lithium and other drugs.
Although rapid cycling has been considered by some to be an “end stage” of the
disorder, empirical evidence indicates that it may have its onset at any time
during the disorder and may come and go during the course of illness. Several
specific risk factors may be associated with rapid cycling, each of which may
give clues to its pathophysiology. These include female gender, anti-depressant
use and prior or current hypothyroidism
History, Physical Examination and Laboratory Studies
Although the diagnosis of manic–depressive disorder is made on the basis
of phenomenology, there are several reasons to con-duct a thorough medical
history and physical examination. First, there are several general medical or
substance-related causes of manic depression that, if treated, may lead to the
resolution of the mood episode. Similarly, mania may be the first sign of a
general medical illness that will be progressive and serious in its own right.
Secondly, medical evaluation is necessary before starting medications used in
the treatment of manic–depressive disorder. Finally, for many patients with
psychiatric illnesses, particularly chronic or severe illnesses, their first
contact with medical care as an adult is during the psychiatric interview,
often under inpa-tient or even involuntary conditions. Because psychiatric
illness is clearly not protective
against medical illnesses, and since even common general medical illnesses may
never have been screened for in the past, a thorough medical history and
physical examina-tion are necessary parts of the basic care of patients.
The overall approach to evaluating persons with manic– depressive
disorder for medical problems may be generalized asfollows: persons with psychiatric
disorders, including manic– depressive disorder, should have regular screening
for disease detection and health maintenance purposes as recommended for the
general population. However, it should also be kept in mind that individuals
with manic–depressive disorder, by virtue of having an often severe and
disabling behavioral disorder, are less likely than the general population to
have had adequate medical screening and treatment. Thus, special care must be
made to en-sure that health problems are not overlooked and that appropriate
treatment or referral is effected. Unfortunately, it is the exception rather
than the rule to have well-integrated medical and mental health systems so that
the mental health provider can assume that some effort will need to be expended
to ensure adequate care is delivered for individuals with manic–depressive
disorder.
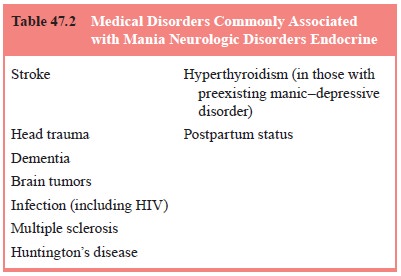
Which general medical illnesses may cause symptoms of manic–depressive
disorder? Most medical illnesses that affect brain function have been described
in case reports or small case series to cause one or another psychiatric
syndrome. Several gen-eral medical illnesses have been associated with the
development of manic–depressive disorder (Table 47.2) although none can be
considered specific risk factors. Administration of medications has been
observed frequently in clinical practice to be associated with the onset of
mania, particularly in patients with preexisting depression. Such medications
are listed in Table 47.3.
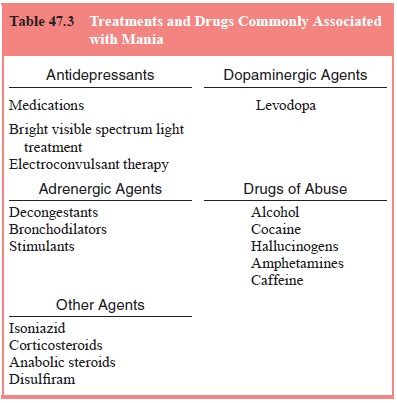
Some controversies have been hotly debated, particularly regarding the
role of antidepressants in causing mania and rapid cycling. Of particular
importance to psychiatric practice, all ef-ficacious antidepressant treatments
have been suspected to cause the induction of mania, with the exception of
lithium and the pos-sible exception of psychotherapy. This caveat for
antidepressants also includes nonpharmacological antidepressants such as light
and electroconvulsive therapy (ECT). The latter effect is para-doxical, as ECT
is also used successfully to treat mania
Related Topics