Chapter: Modern Pharmacology with Clinical Applications: Uterine Stimulants and Relaxants
Uterine Stimulants and Relaxants
Uterine Stimulants and Relaxants
The physiological processes
involved in parturition (i.e., labor,
delivery, and birth) require a complex inter-play of hormonal action, neuronal
activity, and uterine smooth muscle contraction. During the first two
trimesters of pregnancy, the uterus remains in a rela-tively quiescent state,
demonstrating little or no con-traction of the myometrium. This inactivity is
largely the result of the inhibitory action of high circulating levels of
progesterone on the uterine musculature . During the final trimester, however,
uter-ine smooth muscle becomes increasingly excitable, such that mild muscle
contractions are seen (Braxton-Hicks contractions); these gradually increase in
both strength and frequency, occasionally to the extent that they may even be
thought to signal the onset of labor, a phenom-enon termed false labor. Parturition requires in part the integration of
processes that involve cervical canal dila-tion and uterine smooth muscle
contractions that are strong enough to expel the fetus.
Other physiological events
must occur at the end of pregnancy to facilitate birth. The cervix begins to
soften (cervical ripening) as a
direct result of connective tissue dissociation; this process may involve the
actions of the peptide hormone relaxin,
which is produced both in the corpus luteum and in the placenta. Relaxin also
aids in the dissociation of the connective tissue between the pelvic bones, a
process that also aids in the facilitation of birth. At the true onset of
labor, coordinated, rhyth-mic contractions of the uterus begin, and as labor
pro-gresses, the myometrial contractions increase in inten-sity and strength.
These contractions force the fetus against the cervix, further dilating the
cervix. Once the cervix has dilated sufficiently, the uterine contractions push
the fetus through the birth canal.
A variety of endocrine
hormones play a role in ini-tiating the changes in uterine contractility,
especially during the final trimester. It is probable that the con-centration
of receptors responsive to the hypothalamic peptide hormone oxytocin
increases in the uterine musculature in response to the increasing
levels of estrogen during pregnancy. Although circulat-ing blood levels of
oxytocin do not change markedly throughout pregnancy, it is likely that the
augmented number of oxytocin receptors in the uterus makes the muscle
increasingly responsive to plasma oxytocin. There also is speculation that the
uterus itself may be capable of synthesizing oxytocin. If such a synthesis does
indeed occur, much higher local concentrations of the peptide will be found
than would be predicted strictly on the basis of circulating amounts of the
hor-mone. Increases in the number of myometrial α-adren-ergic and angiotensin receptors also
will increase the sensitivity of these muscle cells to contractile stimuli.
Finally, the possibility of fetal factors playing a role in the initiation of
parturition should be considered.
Although, like other smooth
muscle, the myo-metrium is capable of contraction at any time, it is generally
quiescent throughout most of pregnancy. As pregnancy progresses, spontaneous
repetitive action po-tentials can be seen, but muscle tension will develop only
once these action potentials become synchronized electrical discharges.
Contractions do become evident, however, several weeks before labor begins. The
con-tractions of the myometrium progressively increase during the onset of
labor, in part through the action of a positive neuroendocrine feedback system
that in-volves both synthesis and release of oxytocin and
prostaglandins. The stretching
of the softened cervix in-duced by increasing fetal pressure results in local
recep-tor stimulation and the initiating of a spinal reflex that eventually
results in the release of oxytocin from the posterior pituitary. This
additional oxytocin will further promote uterine contractions.
Release of oxytocin at this stage of parturition pro-motes
prostaglandin production, particularly of the E and
F series, within the decidua; these prostaglandins are powerful myometrial
stimulants and thus further enhance uterine contractions. The prostaglandin
con-centration in maternal serum and amniotic fluid in-creases with the
progression of labor.
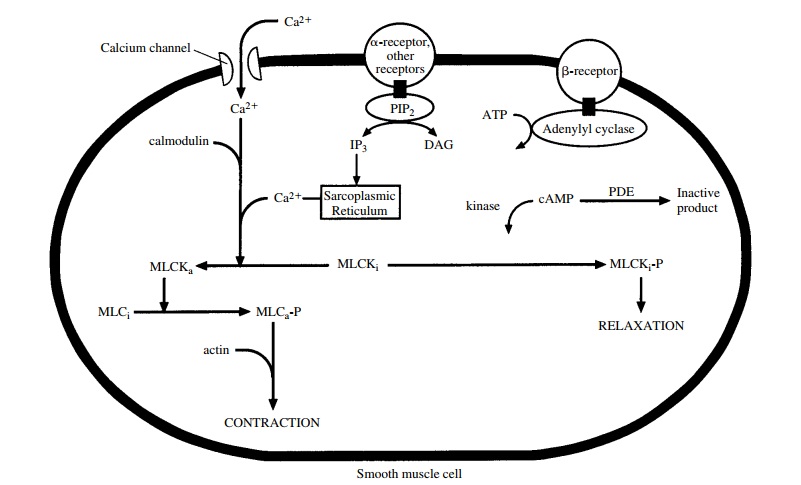
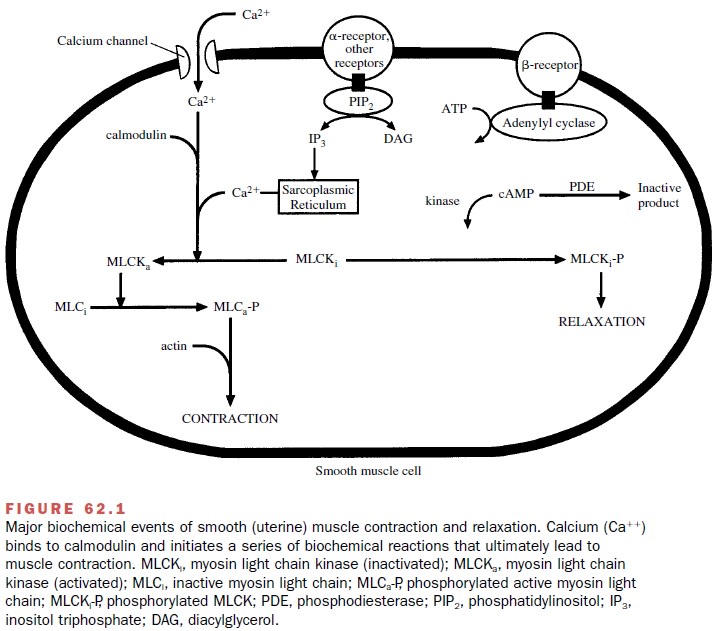
Many of the biochemical and molecular events that are responsible for uterine smooth muscle contraction are the same as those that control other smooth muscle tissues (Fig. 62.1). Once uterine smooth muscle sensitiv-ity has been augmented, actin and myosin must interact for contraction to occur. This interaction depends on the phosphorylation of the contractile proteins by the en-zyme myosin light chain kinase (MLCK). This enzyme requires Ca++ and is active only when associated with calmodulin. Activation of the entire muscle contraction process involves the receptor binding of estrogen, oxy-tocin, α1α-adrenergic agonists, and prostaglandins (PGE1 and PGE2).
A
decrease in the progesterone–estrogen ra-tio in the myometrium is also an
important factor in the timing and initiation of labor; this altered ratio may
in-volve increased fetal estrogen production, particularly in the latter weeks
of pregnancy. Cytokines produced by the
fetus are also thought to be
responsible for stimulating uterine
contraction.
Uterine relaxation is
mediated in part through inhi-bition of MLCK. This inhibition results from the
phos-phorylation of MLCK that follows the stimulation of myometrial β-adrenoceptors; relaxation
involves the activity of a cyclic adenosine monophosphate (cAMP) mediated
protein kinase, accumulation of Ca++ in the sarcoplasmic reticulum,
and a decrease in cytoplasmic Ca++ . Other circulating substances
that favor quies-cence of uterine smooth muscle include progesterone, which
increases throughout pregnancy, and possibly prostacyclin. Progesterone’s
action probably involves hyperpolarization of the muscle cell membrane,
reduc-tion of impulse conduction in muscle cells, and in-creased calcium
binding to the sarcoplasmic reticulum.
Drugs and hormones used clinically to enhance uter-ine contractions
are primarily employed either to induce or to augment contractions during labor
and delivery. They have particular value in limiting an extended preg-nancy,
preventing the early rupture of membranes, or aiding placental insufficiency.
Many of these com-pounds also are useful in limiting postpartum hemor-rhage. The primary use of uterine relaxants
(tocolytic agents) is in the
prevention of premature labor. These drugs
act either directly to suppress myometrial smooth muscle contraction or
indirectly to inhibit synthesis or release of the prostaglandins and/or other
endogenous uterine stimulants.
Related Topics