Chapter: Medical Physiology: Blood Types; Transfusion; Tissue and Organ Transplantation
O-A-B Blood Types
O-A-B Blood Types
A and B Antigens—Agglutinogens
Two antigens—type A and type B—occur on the surfaces of the red blood cells in a large proportion of human beings. It is these antigens (also called agglu-tinogens because they often cause blood cell agglutination) that cause mostblood transfusion reactions. Because of the way these agglutinogens are inher-ited, people may have neither of them on their cells, they may have one, or they may have both simultaneously.
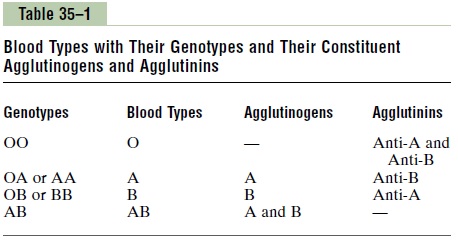
Major O-A-B Blood Types. In transfusing blood from one person to another, thebloods of donors and recipients are normally classified into four major O-A-B blood types, as shown in Table 35–1, depending on the presence or absence of the two agglutinogens, the A and B agglutinogens. When neither A nor B agglu-tinogen is present, the blood is type O. When only type A agglutinogen is present, the blood is type A.When only type B agglutinogen is present, the blood is type B. When both A and B agglutinogens are present, the blood is type Aβ.
Genetic Determination of the Agglutinogens. Two genes, one on each of two pairedchromosomes, determine the O-A-B blood type. These genes can be any one of three types but only one type on each of the two chromosomes: type O, type A,
or type B. The type O gene is either functionless or almost functionless, so that it causes no significant type O agglutinogen on the cells. Conversely, the type A and type B genes do cause strong agglutinogens on the cells.
The six possible combinations of genes, as shown in Table 35–1, are OO, OA, OB, AA, BB, and AB. These combinations of genes are known as the genotypes, and each person is one of the six genotypes.
One can also observe from Table 35–1 that a person with genotype OO produces no agglutinogens, and therefore the blood type is O. A person with genotype OA or AA produces type A agglutinogens and there-fore has blood type A. Genotypes OB and BB give type B blood, and genotype Aβ gives type Aβ blood.
Relative Frequencies of the Different Blood Types.
The prevalence of the different blood types among one group of persons studied was approximately:
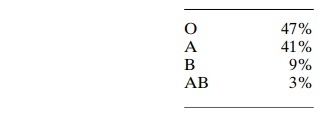
It is obvious from these percentages that the O and A genes occur frequently, whereas the B gene is infrequent.
Agglutinins
When type A agglutinogen is not present in a person’s red blood cells, antibodies known as anti-A agglutinins develop in the plasma. Also, when type B agglutino-gen is not present in the red blood cells, antibodies known as anti-B agglutinins develop in the plasma.
Thus, referring once again to Table 35–1, note that type O blood, although containing no agglutinogens, does contain both anti-A andanti-B agglutinins; type A blood contains type A agglutinogens and anti-Bagglutinins; type B blood contains type B agglutino-gens and anti-A agglutinins. Finally, type Aβ blood contains both A and B agglutinogens but no agglutinins.
Titer of the Agglutinins at Different Ages. Immediately afterbirth, the quantity of agglutinins in the plasma is almost zero. Two to 8 months after birth, an infant begins to produce agglutinins—anti-A agglutinins
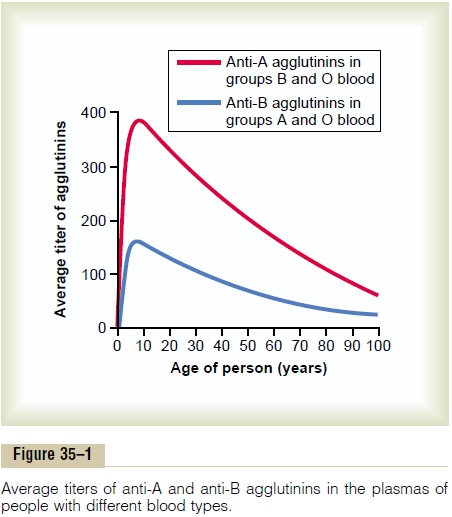
when type A agglutinogens are not present in the cells, and anti-B agglutinins when type B agglutinogens are not in the cells. Figure 35–1 shows the changing titers of the anti-A and anti-B agglutinins at different ages. A maximum titer is usually reached at 8 to 10 years of age, and this gradually declines throughout the remaining years of life.
Origin of Agglutinins in the Plasma. The agglutinins aregamma globulins, as are almost all antibodies, and they are produced by the same bone marrow and lymph gland cells that produce antibodies to any other anti-gens. Most of them are IgM and IgG immunoglobulin molecules.
But why are these agglutinins produced in people who do not have the respective agglutinogens in their red blood cells? The answer to this is that small amounts of type A and B antigens enter the body in food, in bacteria, and in other ways, and these sub-stances initiate the development of the anti-A and anti-B agglutinins.
For instance, infusion of group A antigen into a recipient having a non-A blood type causes a typical immune response with formation of greater quantities of anti-A agglutinins than ever. Also, the neonate has few, if any, agglutinins, showing that agglutinin forma-tion occurs almost entirely after birth.
Agglutination Process In Transfusion Reactions
When bloods are mismatched so that anti-A or anti-B plasma agglutinins are mixed with red blood cells that contain A or B agglutinogens, respectively, the red cells agglutinate as a result of the agglutinins’ attach-ing themselves to the red blood cells. Because the agglutinins have two binding sites (IgG type) or 10 binding sites (IgM type), a single agglutinin can attach to two or more red blood cells at the same time, thereby causing the cells to be bound together by the agglutinin. This causes the cells to clump, which is the process of “agglutination.” Then these clumps plug small blood vessels throughout the circulatory system. During ensuing hours to days, either physical distor-tion of the cells or attack by phagocytic white blood cells destroys the membranes of the agglutinated cells, releasing hemoglobin into the plasma, which is called “hemolysis” of the red blood cells.
Acute Hemolysis Occursin Some Transfusion Reactions.
Sometimes, when recipient and donor bloods are mis-matched, immediate hemolysis of red cells occurs in the circulating blood. In this case, the antibodies cause lysis of the red blood cells by activating the comple-ment system, which releases proteolytic enzymes (the lytic complex) that rupture the cell membranes. Immediate intravascular hemolysis is far less common than agglutination fol-lowed by delayed hemolysis, because not only does there have to be a high titer of antibodies for lysis to occur, but also a different type of antibody seems to be required, mainly the IgM antibodies; these anti-bodies are called hemolysins.
Blood Typing
Before giving a transfusion to a person, it is necessary to determine the blood type of the recipient’s blood and the blood type of the donor blood so that the bloods can be appropriately matched. This is called blood typing and blood matching, and these are per-formed in the following way: The red blood cells are first separated from the plasma and diluted with saline. One portion is then mixed with anti-A agglutinin and another portion with anti-B agglutinin. After several minutes, the mixtures are observed under a micro-scope. If the red blood cells have become clumped— that is, “agglutinated”—one knows that an antibody-antigen reaction has resulted.
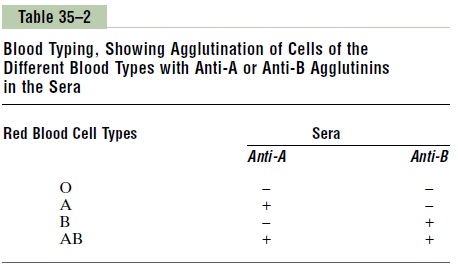
Table 35–2 lists the presence (+) or absence (-) of agglutination of the four types of red blood cells. Type O red blood cells have no agglutinogens and therefore do not react with either the anti-A or the anti-B agglu-tinins. Type A blood has A agglutinogens and there-fore agglutinates with anti-A agglutinins. Type B blood has B agglutinogens and agglutinates with anti-B agglutinins. Type Aβ blood has both A and B agglutinogens and agglutinates with both types of agglutinins.
Related Topics