Chapter: Clinical Cases in Anesthesia : Tracheoesophageal Fistula
How is the patient with a TEF managed intraoperatively?
How is
the patient with a TEF managed intraoperatively?
The optimal surgical management is a one-stage
repair, where the fistula is ligated and the proximal and distal ends of the
esophagus are primarily anastomosed. The approach is typically through a right
thoracotomy incision, with the patient in the left lateral decubitus position.
In the presence of a right aortic arch, a left thoracotomy may be performed.
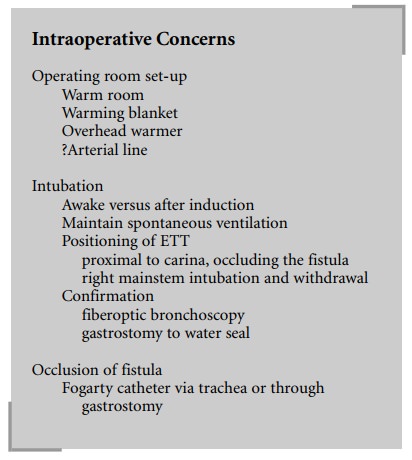
The anesthetic management includes warming of
the operating room and the use of a warming blanket and a radiant overhead
warmer. Standard monitors are applied. An intravenous catheter is placed prior
to induction, if one is not already present. An arterial catheter may be
necessary in high-risk infants. A precordial stethoscope should be securely
positioned in the left axilla for detection of intra-operative airway
obstruction. The esophageal pouch is suctioned and the patient is preoxygenated.
Atropine 0.02 mg/kg may be administered intravenously to prevent bradycardia
during laryngoscopy.
A gastrostomy tube may be placed to decompress
the stomach. However, this may result in a further loss of ven-tilation through
the fistula during positive pressure venti-lation, necessitating clamping of
the gastrostomy tube. Once a common practice, a gastrostomy tube is usually not
placed nowadays, as it may increase the incidence of gastro-esophageal reflux
later in life. If a gastrostomy is per-formed, it is usually accomplished under
local anesthesia prior to induction. It can then be used to aid in the
place-ment of the endotracheal tube (ETT). If the gastric disten-tion does not
impair ventilation, the surgeon may perform the gastrostomy after induction of
general anesthesia.
The optimal anesthetic management of these
patients is to maintain spontaneous ventilation until the fistula is ligated.
Positive pressure ventilation is avoided because it can result in insufflation
of the stomach via the fistula or loss of ventilation through the gastrostomy.
Gastric disten-tion may compromise ventilation and may also lead to aspiration
of gastric contents via the fistula. However, it is not always feasible to
maintain spontaneous ventilation.
Awake intubation is the safest approach. It
allows airway reflexes to be maintained and also allows appropriate
posi-tioning of the ETT without positive pressure ventilation. The
administration of supplemental oxygen during laryn-goscopy can be achieved with
the use of an oxyscope. Awake intubation, however, may be difficult and
traumatic in a vigorous infant. Alternatively, an inhalation or intravenous
induction may be performed without muscle relaxation, thus allowing the infant
to continue to breathe spontaneously.
If a
muscle relaxant is used, care must be taken during positive pressure
ventilation to avoid excessive insufflation of the stomach via the fistula.
Placement and positioning of the ETT can be
tricky. To avoid intubating the fistula, which is located on the poste-rior
aspect of the trachea, the ETT should be inserted with the bevel facing
posteriorly. After intubation, the bevel is rotated anteriorly to avoid
ventilating the fistula.
Since the fistula is usually located just
proximal to the carina, positioning the ETT so that it is above the carina but
still occluding the fistula may be difficult. One com-monly used method is to
insert the ETT (without a Murphy eye) into the right mainstem bronchus and then
gradually withdraw it until breath sounds are heard on the left. However, this
does not always assure that the endotracheal tube occludes the fistula. If a
gastrostomy tube is in place, the distal end is submerged in a beaker of water
and if bubbling occurs there is leakage through the fistula. The ETT is then
advanced until the bubbling ceases while still maintaining left-sided breath
sounds. The gastrostomy tube may be left to water seal during the surgery,
which allows for continued monitoring for ventilation through the fistula.
A second method of confirming placement of the
ETT is with the use of a fiberoptic bronchoscope. After intuba-tion, the
fiberoptic bronchoscope is passed through the ETT and the carina is visualized.
Upon withdrawal of the bronchoscope, if the fistula is not visualized then the
ETT is appropriately positioned. If the fistula is visualized, the ETT is
advanced making sure that its tip remains above the carina.
Sometimes, with a large fistula or one that is
located at or distal to the carina, placement of the ETT to avoid ventilating
the fistula is not possible. In this situation, the fistula may need to be
occluded with a Fogerty balloon catheter placed from above with the help of a
broncho-scope or from below through the gastrostomy.
Once positioned, the ETT should be carefully
secured. After the patient is positioned in the left lateral decubitus
position, reconfirmation of the position of the ETT may be necessary.
Loss of breath sounds and the end-tidal carbon
dioxide (ETCO2) tracing commonly occurs during surgery second-ary to
airway obstruction. This may be due to the accumu-lation of secretions or blood
in the ETT. More often, however, it results from kinking of the trachea during
sur-gical manipulation. The surgeon should immediately be instructed to release
the surgical traction.
Related Topics