Chapter: Medical Microbiology: An Introduction to Infectious Diseases: Eye, Ear, and Sinus Infections
Ear Infections
EAR INFECTIONS
Most infections of the ear involve the external otic canal (otitis externa) or the middle ear cavity (otitis media), which contains the ossicles and is enclosed by bony structures and the tympanic membrane. Factors of importance in the pathogenesis of otitis externa in-clude local trauma, furunculosis, foreign bodies, or excessive moisture, which can lead to maceration of the external ear epithelium (swimmer’s ear). Occasionally, external otitis occurs as an extension of infection from the middle ear, with purulent drainage through a perforated tympanic membrane.
The eustachian tube, which vents the middle ear to the nasopharynx, appears to play a major role in predisposing patients to otitis media. The tube performs three functions: ventilation, protection, and clearance via mucociliary transport. Viral upper respiratory in-fections or allergic conditions can cause inflammation and edema in the eustachian tube or at its orifice. These developments disturb its functions, of which ventilation may be the most important. As ventilation is lost, oxygen is absorbed from the air in the middle ear cavity, producing negative pressure. This pressure in turn allows entry of potentially path-ogenic bacteria from the nasopharynx into the middle ear, and failure to clear these nor-mally can result in colonization and infection. Other factors that can lead to compromise of eustachian tube function include anatomic abnormalities, such as tissue hypertrophy or scarring around the orifice, muscular dysfunction associated with cleft palate, and lack of stiffness of the tube wall. The latter is common in infancy and early childhood and im-proves with age. It may explain in part why otitis media occurs most often in infants 6 to 18 months of age and then decreases in frequency as patency of the eustachian tube be-comes established.
MANIFESTATIONS
Otitis externa is characterized by inflammation of the ear canal, with purulent ear drainage. It can be quite painful, and cellulitis can extend into adjacent soft tissues. A common form is associated with swimming in water that may be contaminated with aerobic, Gram-nega-tive organisms such as Pseudomonas species. “Malignant” otitis externa is a considerably more severe form of external ear canal infection that can progress to invasion of cartilage and adjacent bone, sometimes leading to cranial nerve palsy and death. It is seen most fre-quently in elderly patients with diabetes mellitus and in immunocompromised hosts of any age. Pseudomonas aeruginosa is the most common causative pathogen.
Otitis media is arbitrarily classified as acute, chronic, or serous (secretory). Acute oti-tis media, nearly always caused by bacteria, is often a complication of acute viral upper respiratory illness. Fever, irritability, and acute pain are common, and otoscopic examina-tion reveals bulging of the tympanic membrane, poor mobility, and obscuration of normal anatomic landmarks by fluid and inflammatory cells under pressure. In some cases, the tympanic membrane is also acutely inflamed, with blisters (bullae) on its external surface (myringitis). If treated inadequately, the infection can progress to involve adjacent struc-tures such as the mastoid air cells (mastoiditis) or lead to perforation with spontaneous drainage through the tympanic membrane. Potential acute, suppurative sequelae include extension into the central nervous system (CNS) and sepsis.
Chronic otitis media is usually a result of acute infection that has not resolved ade-quately, either because of inadequate treatment in the acute phase or because of host fac-tors that perpetuate the inflammatory process (eg, continued eustachian tube dysfunction, caused by allergic or anatomic factors or immunodeficiency). Sequelae include progres-sive destruction of middle ear structures and a significant risk of permanent hearing loss. Serous otitis media may represent either a form of chronic otitis media or allergy-related inflammation. It tends to be chronic, causing hearing deficits, and is associated with thick, usually nonpurulent secretions in the middle ear.
COMMON ETIOLOGIC AGENTS
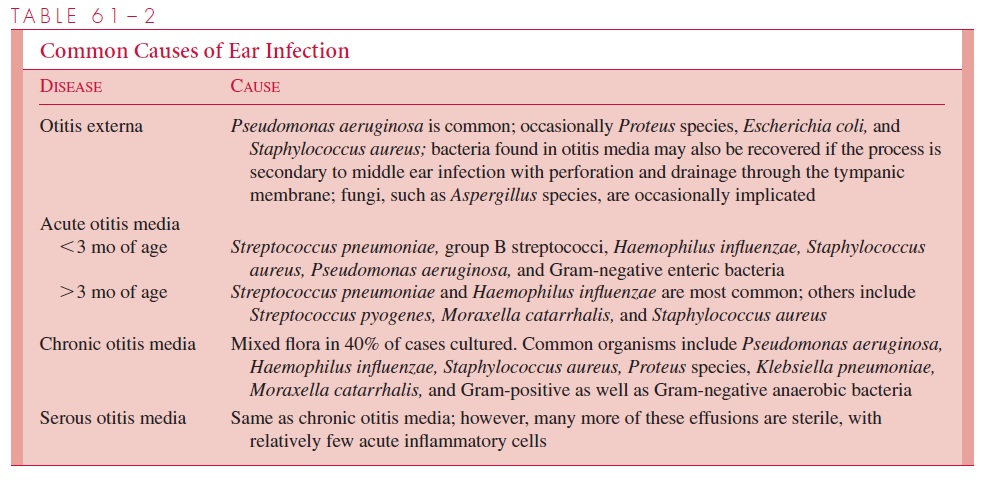
The usual causes of ear infections are listed in Table 61 – 2. S. pneumoniae is the single most common cause of acute otitis media after the first 3 months of life, accounting for 35 to 40% of all cases. H. influenzae is also common, particularly in patients less than 5 years of age. The majority of H. influenzae isolates from the middle ear are nontypeable; thus the current vaccine against type b strains would not be expected to markedly reduce the incidence of acute otitis media. Viruses and Mycoplasma are rare primary causes of acute or chronic otitis media; however, they predispose patients to superinfection by the bacterial agents.
DIAGNOSTIC APPROACHES
The diagnosis is established on the basis of clinical examination. Tympanometry can be performed in suspected cases of otitis media to detect the presence of fluid in the middle ear and to assess tympanic membrane function.
The specific etiology of otitis externa can be determined by culture of the affected ear canal; however, one must keep in mind that surface contamination and normal skin flora may lead to mixed cultures, which can be confusing. In otitis media, the most precise diagnostic method is careful aspiration with a sterile needle through the tympanic membrane after decontamination of the external canal. Gram stain and culture of such aspirates is highly reliable; however, this procedure is generally reserved for cases in which etiologic possibilities are extremely varied, as in young infants, or when clinical response to the usual antimicrobial therapy has been inad-equate. Respiratory tract cultures, such as those from the nasopharynx, cannot be relied on to provide an etiologic diagnosis.
MANAGEMENT PRINCIPLES
Except in severe cases, otitis externa can usually be managed by gentle cleansing with topical solutions. The Gram-negative bacteria most commonly involved are often suscep-tible to an acidic environment, and otic solutions buffered to a low pH (3.0 or less), as with 0.25% acetic acid, are often effective. Various preparations are available, many of which also contain antimicrobics.
Acute otitis media requires antimicrobial therapy and careful follow-up to ensure that the disease has resolved. The choice of antimicrobic is usually empirical, designed specifi-cally to cover the most likely bacterial pathogens, because direct aspiration for diagnostic purposes is usually unnecessary. In the usual case, these pathogens would be S. pneumoniae and H. influenzae. If there is extreme pressure with severe pain, drainage of middle ear exudates by careful incision of the tympanic membrane may be necessary. In patients with chronic or serous otitis media, management can be more complex, and it is often advisable to seek otolaryngologic consultation to determine further diagnostic procedures as well as to plan medical and possible surgical measures.
Related Topics