Chapter: Clinical Cases in Anesthesia : Mitral Stenosis
What is the etiology and pathophysiology of mitral stenosis?
What is
the etiology and pathophysiology of mitral stenosis?
Mitral stenosis is frequently rheumatic in
origin. In many patients, there is a latency period of 30–40 years between the
episode of rheumatic fever and the onset of clinical symptoms. Dyspnea is the
most common symp-tom. The initial presentation is often due to an episode of
atrial fibrillation or to an unrelated condition, such as preg-nancy,
thyrotoxicosis, anemia, or sepsis. Other common symptoms include fatigue,
palpitations, or hemoptysis.
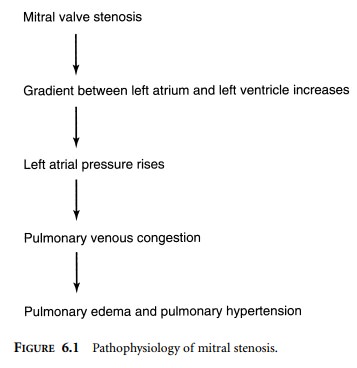
In the normal adult, the mitral valve orifice
is 4–6 cm2. As the orifice narrows, to less than 2 cm2,
the pressure gradient between the left atrium and left ventricle must increase
to maintain adequate flow. The high left atrial pressure causes pulmonary
venous congestion, which eventually leads to pulmonary edema, particularly in
the presence of tachycardia (Figure 6.1). Tachycardia shortens diastole and
diminishes the time available for flow across the mitral valve. This, in turn,
impairs left atrial emptying and left ventricular filling. Cardiac output
decreases, pulmonary congestion increases, and decompensation ensues. A mitral
valve area less than 1.0 cm2 is considered critical. The decision to
perform valve surgery, however, is usually based on the severity of symp-toms
(i.e., New York Heart Association Classification).
Although the left ventricle is “protected” from pressure or volume overload, left ventricular contractility may be impaired by rheumatic involvement of the
papillary muscles and mitral annulus. Left ventricular function might also be
impaired by a shift of the interventricular septum due to right ventricular
(RV) pressure overload. Pulmonary hyper-tension and RV failure are often
observed in mitral stenosis.
Related Topics