Chapter: Essentials of Psychiatry: Mood Disorders: Bipolar (Manic–Depressive) Disorders
Episodes as the Basis for Diagnosis of Manic–Depressive Disorder
Episodes as the Basis for Diagnosis of Manic–Depressive
Disorder
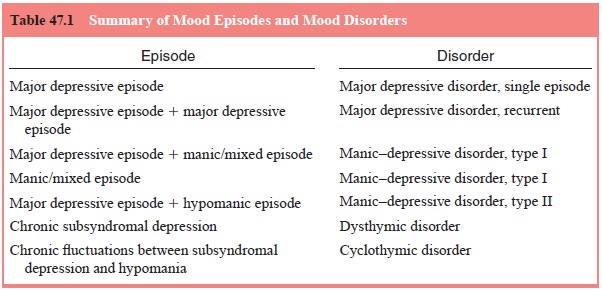
The DSM-based definition of manic–depressive disorder is built on the
identification of individual mood episodes
(Table 47.1). DSM-IV criteria for individual mood episodes are summarized below
for manic, mixed and hypomanic episodes. Criteria for these episodes are
reviewed in greater detail in the subsequent section on diagnosis. It is
important to understand that the di-agnosis of manic–depressive disorder
derives from the occur-rence of individual episodes over time. Persons who
experience a manic, hypomanic, or mixed episode, virtually all of whom also
have a history of one or more major depressive episodes, are di-agnosed with
manic–depressive disorder. Those who experience major depressive and manic
episodes are diagnosed with bipo-lar I disorder,
and those with major depressive and hypomanic (milder manic) episodes are diagnosed with bipolar II disorder.
Not surprisingly, most data regarding manic–depressive disorder come
from the study of the more severe end of the spec-trum, primarily type I
disorder. Throughout this, data on manic–depressive disorder derive from
studies of type I disorder unless otherwise noted. DSM-IV-TR is the first
version of the DSM series to include a specific category for bipolar II
disor-der. Previously, persons with depressive and hypomanic episodes were
grouped under the broad “bipolar disorder not otherwise specified”, which
included a variety of unusual presentations.
Study of the course over time of type II disorder indicated that persons
with hypomania tended to have recurrent hypomanic episodes and did not convert
into type I by developing mania. In ad-dition, persons with type II disorder
may have more episodes overtime than persons with type I indicating that the
course of type II differs from that of type I. However, biological differences
between these manic–depressive types have not been reliably demonstrated.
However, it should not be construed that manic–depressive disor-der type II is
in all respects milder than type I, although hypomania is by definition less severe
than mania. Specifically, the social and occupational function and quality of
life for persons with type II disorder are similar to those for persons with
type I disorder.
Persons who experience subsyndromal manic–depressive mood fluctuations
over an extended period without major mood episodes are diagnosed with cyclothymic disorder. Much less is
known about this milder disorder because afflicted persons present for medical
attention less frequently than those with full-blown manic–depressive disorder.
Cyclothymic disorder has been considered at various times a temperament, a
personality disor-der and a disorder at the milder end of the manic–depressive.
DSM-IV-TR Criteria 301.13
Etiology and Pathophysiology
It is clear from current data that no single paradigm can explain the
occurrence, and variability in course and severity of manic– depressive
disorder. Rather, a more integrative approach to un-derstanding the causes of
manic–depressive disorder is needed, one which recognizes the contributions of
varying degrees of importance from several sources.
Further, in trying to understand the source of symptoms at a particular
time in a particular person with manic–depres-sive disorder we must keep in
mind that there may be multiple sources that lead to the symptoms that we are
trying to treat. It is not likely that biological theories will explain all the
pathology seen in manic–depressive disorder. Similarly, the effectiveness of
medications such as lithium renders purely psychosocial theories untenable. An
integrative biopsychosocial mindset
will likely be the most successful approach to treatment, as Engel articulated
for all illnesses, both medical and psychiatric.
Related Topics