Chapter: Obstetrics and Gynecology: The Obstetrician-Gynecologist’s Role in Screening and Preventive Care
Colorectal Carcinoma
CERVICAL CANCER
Cervical
intraepithelial neoplasia (CIN) is the precur-sor lesion to
cervical cancer. CIN may regress sponta-neously, but, in some cases, CIN 2 and
CIN 3 progresses to cancer over time. Exfoliative cytology,specifically thePap test (either slide or liquid-based) with or without
type-specific HPV identification, allow early diagnosis in most cases. The
reduction in mortality from cervical cancer since the Pap test was introduced
in the 1940s is testimony to the success of this screening program.
The following are recommendations
for cervical can-cer screening for women:
·
Annual cervical cytology
screening should begin ap-proximately 3 years after initiation of sexual
inter-course, but no later than age 21 years. Women younger than 30 years
should undergo annual cervical cytology screening.
·
Women who have had 3 consecutive
negative annual Pap test results may be screened every 2 to 3 years if they are
age 30 or older with no history of CIN 2 or 3, immunosuppression, HIV
infection, or diethylstilbes-trol (DES) exposure in utero. Annual cervical
cytology is another option for women 30 years and older. The use of combination
cervical cytology and human papil-lomavirus (HPV) DNA screening is appropriate
for women 30 years and older. Women who receive nega-tive results on both tests
should be rescreened no more frequently than every 3 years.
·
Women who have had a total
hysterectomy (removal of the uterus and cervix) for reasons other than cervical
cancer no longer need to be screened for cervical cancer. Women who have had a
supracervical hysterectomy should continue to be screened. Women who have
undergone hysterectomy with removal of the cervix and have a history of CIN 2
or CIN 3 should continue to be screened annually until three consecutive
negative vagi-nal cytology test results are achieved.
COLORECTAL CARCINOMA
With over 75,000 new cases of colorectal cancer annu-ally in women
and over 25,000 deaths, colorectal cancer is the third leading cause of cancer
death in women, after lung cancer and breast cancer. Because early detection
(preinvasive or early invasive stage) allows effective man-agement for most
patients, screening is appropriate and recommended.
Screening
for colorectal cancer is recommended for all women at average risk, starting at
the age of 50. The preferredmethod is colonoscopy, performed every 10 years.
Other acceptable screening tests
include:
· Annual fecal occult blood testing (FOBT) or fecalimmunochemical testing (FIT)
· Flexible
sigmoidoscopy every 5 years. This test will miss right-sided lesions, which may
account for up to 65% of advanced colorectal cancers in women.
· Combination
of annual fecal occult blood testing and flexible sigmoidoscopy
· Double
contrast barium enema every 5 years
Both FOBT and FIT require two or
three samples of stool collected by the patient at home and returned for
analysis. Screening by FOBT of a single stool sample from a rectal examination
by the physician is not adequate for the de-tection of colorectal cancer and is
not recommended. Dif-ferent recommendations apply to women at increased risk
and at high risk.
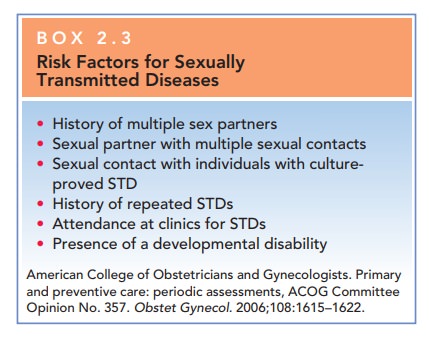
Sexually Transmitted Diseases
Appropriate STD screening in
nonpregnant women de-pends on the age of the patient and the assessment of risk
factors (Box 2.3). Because of the risk that STDs pose in pregnancy, pregnant
women are routinely screened for syphilis, HIV, chlamydia, and gonorrhea.
Related Topics