Chapter: Psychiatric Mental Health Nursing : Anger, Hostility, and Aggression
Applying the Nursing Process - Anger, Hostility, and Aggression
APPLYING THE NURSING PROCESS
Assessment and effective intervention with angry or hos-tile clients can often prevent aggressive episodes. Early assessment, judicious use of medications, and verbal inter-action with an angry client can often prevent anger from escalating into physical aggression.
Assessment
The nurse should be aware of factors that influence aggres-sion in
the psychiatric environment, or unit milieu. Aggres-sive behavior is less
common on psychiatric units with strong psychiatric leadership, clear staff
roles, and planned and adequate events such as staff–client interaction, group
interaction, and activities. Conversely, when predictability of meetings or
groups and staff–client interactionsare lacking, clients often feel frustrated
and bored, and aggression was more common and intense. A lack of psy-chological
space—having no privacy, being unable to get sufficient rest—may be more
important in triggering aggression than a lack of physical space.
In addition to assessing the unit milieu, the nurse needs to assess
individual clients carefully. A history of violent or aggressive behavior is
one of the best predictors of future aggression. Determining how the client
with a history of aggression handles anger and what the client believes is
helpful is important in assisting him or her to control or nonaggressively
manage angry feelings. Clients who are angry and frustrated and believe that no
one is listening to them are more prone to behave in a hostile or aggressive
manner. In addition to a past history of violence, a history of being
personally victimized and one of substance abuse increase a client’s likelihood
of aggressive behavior. Indi-vidual cues can help the nurse recognize when
aggressive behavior is imminent (Pryor, 2005). These cues include what the
client is saying; changes in the client’s voice— volume, pitch, speed; changes
in the client’s facial expres-sion; and changes in the client’s behavior.
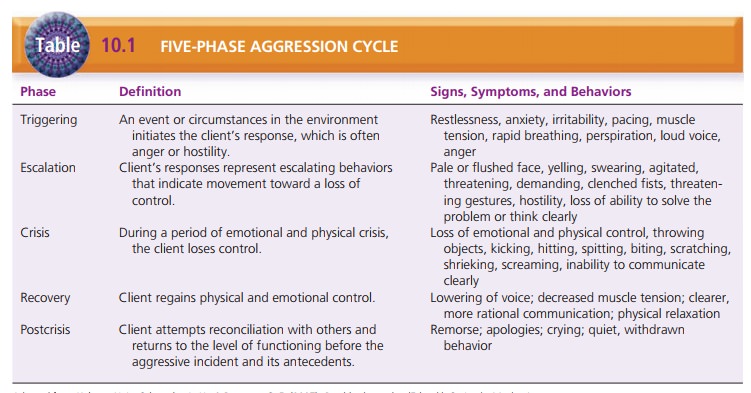
The nurse should assess the client’s behavior to deter-mine which
phase of the aggression cycle he or she is in so that appropriate interventions
can be implemented. The five phases of aggression and their signs, symptoms,
and behaviors are presented in Table 10.1. Assessment of cli-ents must take
place at a safe distance. The nurse can approach the client while maintaining an
adequate distance so that the client does not feel trapped or threatened. To
ensure staff safety and exhibit teamwork, it may be prudent for two staff
members to approach the client.
Data Analysis
Nursing diagnoses commonly used when working with aggressive
clients include the following:
·
Risk for Other-Directed Violence
·
Ineffective Coping
If the client is intoxicated, depressed, or psychotic, addi-tional
nursing diagnoses may be indicated.
Outcome Identification
Expected outcomes for aggressive clients may include the following:
·
The client will not harm or threaten others.
·
The client will refrain from behaviors that are intimi-dating or
frightening to others.
·
The client will describe his or her feelings and concerns without
aggression.
·
The client will comply with treatment.
Intervention
Hostility or verbally aggressive behavior can be intimidat-ing or
frightening even for experienced nurses. Clients exhibiting these behaviors are
also threatening to other cli-ents, staff, and visitors. In social settings,
the most frequent response to hostile people is to get as far away from them as
possible. In the psychiatric setting, however, engaging the hostile person in
dialogue is most effective to prevent the behavior from escalating to physical
aggression.
Interventions are most effective and least restrictive when
implemented early in the cycle of aggression. This section presents
interventions for the management of the milieu (which benefit all clients
regardless of setting) and specific interventions for each phase of the
aggression cycle.
Managing the Environment
It is important to consider the environment for all clients when
trying to reduce or eliminate aggressive behavior. Group and planned activities
such as playing card games, watching and discussing movies, or participating in
informaldiscussions give clients the opportunity to talk about events or issues
when they are calm. Activities also engage clients in the therapeutic process
and minimize boredom. Scheduling one-to-one interactions with clients indicates
the nurse’s genuine interest in the client and a willingness to listen to the
client’s concerns, thoughts, and feelings. Knowing what to expect enhances the
client’s feelings of security.
If clients have a conflict or dispute with one another, the nurse
can offer the opportunity for problem-solving or conflict resolution.
Expressing angry feelings appropri-ately, using assertive communication
statements, and negotiating a solution are important skills clients can
prac-tice. These skills will be useful for the client when he or she returns to
the community.
If a client is psychotic, hyperactive, or intoxicated, the nurse
must consider the safety and security of other clients, who may need protection
from the intrusive or threatening demeanor of that client. Talking with other
clients about their feelings is helpful, and close supervision of the client
who is potentially aggressive is essential.
Managing Aggressive Behavior
In the triggering phase,
the nurse should approach the client in a nonthreatening, calm manner in order
to de-escalate the client’s emotion and behavior. Conveying empathy for the
client’s anger or frustration is important. The nurse can encourage the client
to express his or her angry feelings ver-bally, suggesting that the client is
still in control and can maintain that control. Use of clear, simple, short
statements is helpful. The nurse should allow the client time to express
himself or herself. The nurse can suggest that the client go to a quiet area or
may get assistance to move other clients to decrease stimulation. Medications
(PRN, or as needed) should be offered, if ordered. As the client’s anger
subsides, the nurse can help the client to use relaxation techniques and look
at ways to solve any problem or conflict that may exist (Marder, 2006).
Physical activity, such as walking, also may help the client relax and become
calmer.
If these techniques are unsuccessful and the client pro-gresses to
the escalation phase (period when
client builds toward loss of control),
the nurse must take control of thesituation. The nurse should provide
directions to the client in a calm, firm voice. The client should be directed
to take a time-out for cooling off in a quiet area or his or her room. The
nurse should tell the client that aggressive behavior is not acceptable and
that the nurse is there to help the client regain control. If the client
refused medications during the triggering phase, the nurse should offer them
again.
If the client’s behavior continues to escalate and he or she is
unwilling to accept direction to a quiet area, the nurse should obtain
assistance from other staff members. Initially, four to six staff members
should remain ready within sight of the client but not as close as the primary
nurse talking with the client. This technique, sometimes called a “show of
force,” indicates to the client that the staff will control the situation if
the client cannot do so. Sometimes the presence of additional staff convinces
the client to accept medication and take the time-out necessary to regain
control.
When the client becomes physically aggressive (crisis phase), the staff
must take charge of the situation for the
safety of the client, staff, and other clients. Psychiatric facilities
offer training and practice in safe techniques for managing behavioral
emergencies, and only staff with such training should participate in the
restraint of a physi-cally aggressive client. The nurse’s decision to use seclu-sion
or restraint should be based on the facility’s protocols and standards for
restraint and seclusion. The nurse should obtain a physician’s order as soon as
possible after decid-ing to use restraint or seclusion.
Four to six trained staff members are needed to restrain an
aggressive client safely. Children, adolescents, and female clients can be just
as aggressive as adult male clients. The client is informed that his or her
behavior is out of control and that the staff is taking control to provide safety
and pre-vent injury. Four staff members each take a limb, one staff member
protects the client’s head, and one staff member helps control the client’s
torso, if needed. The client is trans-ported by gurney or carried to a
seclusion room, and restraints are applied to each limb and fastened to the bed
frame. If PRN medication has not been taken earlier, the nurse may obtain an
order for intramuscular (IM) medication in this type of emergency situation. As
notedpreviously, the nurse performs close assessment of the client in seclusion
or restraint and documents the actions.
As the client regains control (recovery
phase), he or she is encouraged to talk about the situation or triggers
that led to the aggressive behavior. The nurse should help the client relax,
perhaps sleep, and return to a calmer state. It is important to help the client
explore alternatives to aggressive behavior by asking what the client or staff
can do next time to avoid an aggressive episode. The nurse also should assess
staff members for any injuries and com-plete the required documentation such as
incident reports and flow sheets. The staff usually has a debriefing session to
discuss the aggressive episode, how it was handled, what worked well or needed
improvement, and how the situation could have been defused more effectively. It
also is important to encourage other clients to talk about their feelings
regarding the incident. However, the aggressive client should not be discussed
in detail with other clients.
In the postcrisis phase, the client is removed from restraint
or seclusion as soon as he or she meets the behavioral criteria. The nurse
should not lecture or chastise the client for the aggressive behavior but
should discuss the behavior in a calm, rational manner. The client can be given
feedback for regaining control, with the expectation that he or she will be
able to handle feelings or events in a nonaggressive manner in the future. The
client should be reintegrated into the milieu and its activities as soon as he
or she can participate.
Evaluation
Care is most effective when the client’s anger can be defused in an
earlier stage, but restraint or seclusion is sometimes necessary to handle
physically aggressive behavior. The goal is to teach angry, hostile, and
potentially aggressive clients to express their feelings verbally and safely
without threats or harm to others or destruction of property.
Related Topics