Chapter: Essentials of Psychiatry: Physician–Patient Relationship
Special Issues in the Physician–Patient Relationship
Special Issues in the
Physician–Patient Relationship
Phase of Treatment
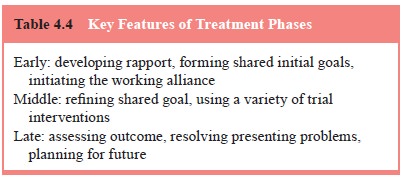
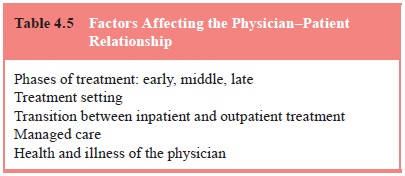
The treatment phase – early, middle, or late (Table
4.4) – affects the structure of the physician–patient relationship in terms of
both the issues to be addressed and the task to be accomplished by the
physician and the patient. The early stage of treatment involves developing a
rapport, forming shared initial goals, and initiating the working alliance.
Education of the patient is important to the success of the physician–patient
relationship in this stage, so that the patient learns what he or she can
expect. In the middle stage of treatment, the physician and patient
continuously refine their shared goals, and various interventions are tried.
While this takes place, transference and countertransference are likely to
emerge. How these are recognized and managed is critical to whether the
relationship continues and is therapeutic.
In the later phase of treatment, the assessment of
the out-come and plans for the future are the primary focus. The phy-sician and
the patient discuss the end of their relationship in a process known as
termination. Successes and disappointments associated with the treatment are
reviewed. The physician must be willing to acknowledge the patient’s
disappointments, as well as recognize her or his own disappointments in the treatment.
The therapeutic alliance is strengthened in this stage when the physician
accepts expressions of the patient’s disappointments, encourages such
expressions when they are not forthcoming,
and prepares the patient for the future. Such
preparations in-clude orienting the patient as to when he or she might seek
fur-ther treatment (Ursano and Silberman, 2002). Solidifying the
physician–patient relationship at the end of the treatment can be critical to
the patient’s self-esteem and willingness to return if symptoms reappear (Table
4.5).
As a part of the termination process the physician
and the patient must review what has been learned, discuss what changes have
taken place in the patient and the patient’s life, and acknowledge together the
sadness and joy of their leave-taking. The termination involves a mourning
process even when treatment has been brief or unpleasant. Of course, when the
physician–patient relationship has been rewarding, and both physician and
patient are satisfied with what they have accom-plished, mourning is more
intense and often characterized by a bittersweet sadness.
Treatment Settings
The physician–patient relationship takes place in a
variety of treatment settings. These include the private office, community clinic,
emergency room, inpatient psychiatric ward and general hospital ward.
Psychiatrists treating patients in a private office may find that the relative
privacy of this setting enhances the early establishment of trust related to
confidentiality. In addi-tion, the psychiatrist’s personality is more evident
in the private office where personal factors influencing choice of decor, room
arrangement and location play a role. However, in contrast to the hospital or
community setting, the private office generally lacks other evidence of the
physician’s competence and humanness. In hospital and community settings, when
a colleague greets the physician and the patient in the hall, or the physician
receives a call for a consultation by a colleague or for a meeting, it
indicates to the patient that the physician is qualified, skilled and humane.
On the other hand, therapeutic work conducted in
the com-munity clinic, emergency room and general hospital ward often requires
the psychiatrist and patient to adapt rapidly to meeting one another, assessing
the problem, establishing treatment goals, and ensuring the appropriate
interventions and follow-up. The importance of protecting the patient’s needs
for time, predictabil-ity and structure can run counter to the demands of a
busy serv-ice and unexpected clinical and administrative requirements. The
psychiatrist must stay alert to the patient’s perspective but not all
interruptions can be avoided. The patient can be informed and accommodated as
much as possible, and any feelings of hurt, disappointment, or anger can be
listened for by the physician and responded to empathically. At times,
patients, particularly those with borderline personality disorder, may require
transfer to an-other psychiatrist whose schedule can accommodate the patient’s
exquisite needs for stability.
The boundaries of confidentiality are necessarily
extended in hospital and community settings to include consultation withother
physicians, nursing staff and often family members (Wise and Rundell, 2002).
Particular attention must always be given to the patient’s need for and right
to respect and privacy. Regardless of the setting, patients receiving
medication must be fully informed about the potential risks and benefits of and
alternatives to the recommended pharmacological treatment (Kessler, 1991).
Patients must be educated about the risks and benefits of receiv-ing prescribed
treatment and of not receiving treatment. This is an important component of
maintaining the physician–patient relationship. Patients who are informed about
and involved in de-cisions about medication respect the physician’s role and
interest in their welfare. Psychiatrists must also pay particular attention to
the meaning a patient attaches to any prescribed medication, particularly when
the time comes to alter or discontinue its use (Ursano et al., 1991).
The change from inpatient to outpatient therapy
involves the resumption of a greater degree of autonomy by the patient in the
physician–patient dyad. The physician must actively encour-age this separation
and its hope for the future. This transition is delicate for any therapeutic
pair.
Managed Care
Managed care, broadly defined as any care of
patients that is not determined solely by the provider, currently focuses on
the economic aspects of delivering medical care, with little atten-tion thus
far to its potential effects on the physician–patient relationship (Goodman et
al., 1992). Discontinuity of care and the creation of unrealistic expectations
on the part of patients have been raised as likely deleterious effects on that
relation-ship (Emanuel and Brett, 1993). Other issues that can affect the
physician–patient relationship include the erosion of con-fidentiality,
shrinkage of the types of reimbursable services, and diminished autonomy of the
patient and the physician in medical decision-making. Additionally, many
managed care systems dictate a split treatment model, with the psychiatrist
prescribing psychopharmacologic treatment and a separate clinician providing
psychotherapy. In such a system, there are complicated challenges faced both by
clinicians and patients. With neither party in complete control of decisions,
the physi-cian–patient relationship can become increasingly adversarial and
subservient to external issues such as cost, quality of life, political
expediency and social efficiency (Siegler, 1993).
Related Topics