Chapter: Clinical Cases in Anesthesia : Cardiopulmonary Resuscitation
What is the treatment of supraventricular tachydys-rhythmias?
What is
the treatment of supraventricular tachydys-rhythmias?
The most important initial step is to evaluate
whether the patient with an underlying tachycardia is stable or unstable.
Tachycardias in unstable patients require imme-diate electrical cardioversion,
whereas stable tachycardias are usually treated with drugs and/or electric
cardioversion until further evaluation and diagnostic measures can be
performed. It is extremely important to treat all wide com-plex
tachydysrhythmias as VT. Clinical or ECG criteria used to differentiate wide
complex supraventricular tachy-cardias from VT are problematic. Administration
of verapamil to a patient with VT may cause irreversible hemo-dynamic collapse.
However, since adenosine has almost no effect on blood pressure, it can be tried
in stable patients who are suspected of having a wide complex supraventric-ular
tachycardia. Adenosine is an endogenous purine nucleoside that depresses sinus
and AV nodal activity that is extremely short-acting (the serum half-life is
less than 5 seconds) and produces few significant side-effects.
In narrow complex supraventricular
tachycardias, vagal maneuvers should be performed or adenosine (0.1 mg/kg i.v.
push) administered to help identify the exact underlying rhythm. Treatment also
depends on the underlying cardiac function (preserved or impaired, ejection
fraction (EF) <40%, congestive heart failure). Paroxysmal supraventricular
tachy-cardias can be treated with calcium-channel blockers, β-blockers, digoxin, or amiodarone (the latter especially in the patient with impaired cardiac function). In junctional
tachycardia or ectopic or multifocal atrial tachycardia, elec-trical
cardioversion is not recommended.
If atrial fibrillation/flutter is suspected as
the underlying rhythm, it is imperative to evaluate the patient before further
management is initiated. If possible, the patient’s cardiac function should be
assessed, a Wolff-Parkinson-White (WPW) syndrome ruled out, and the time of
onset of atrial fibrillation determined (<48 hours or >48 hours). The
goals are to treat unstable patients urgently to control the rate, convert the
rhythm, and to provide anticoagulation. Patients with an onset of symptoms >
48 hours should be evaluated for thrombi in the atria using transesophageal
echocardiography (TEE) before electric cardioversion is attempted. WPW patients
are preferably treated with elec-tric cardioversion or amiodarone. In these
patients, adeno-sine, β-blockers, calcium-channel blockers, and
digoxin are contraindicated. These drugs can lead to an increased ven-tricular
response or may precipitate VF by selectively blocking the AV node in patients
with coexisting accessory conduction pathways. Once the diagnosis of atrial
fibrilla-tion/flutter is confirmed, treatment usually consists of elec-tric
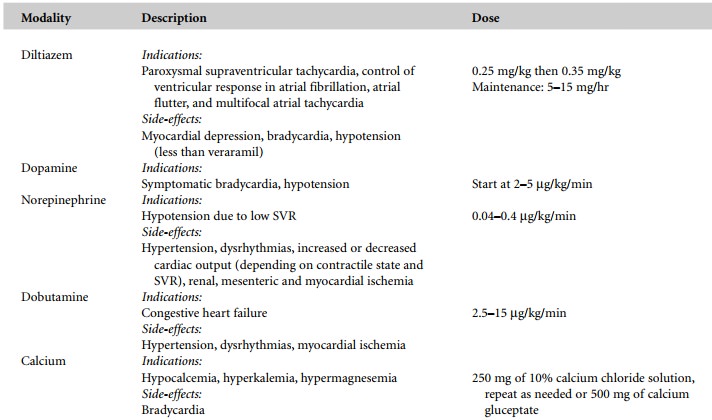
cardioversion, β-blockers, calcium-channel blockers (e.g.,
diltiazem), or digoxin. Amiodarone is preferred in the unstable patient or the
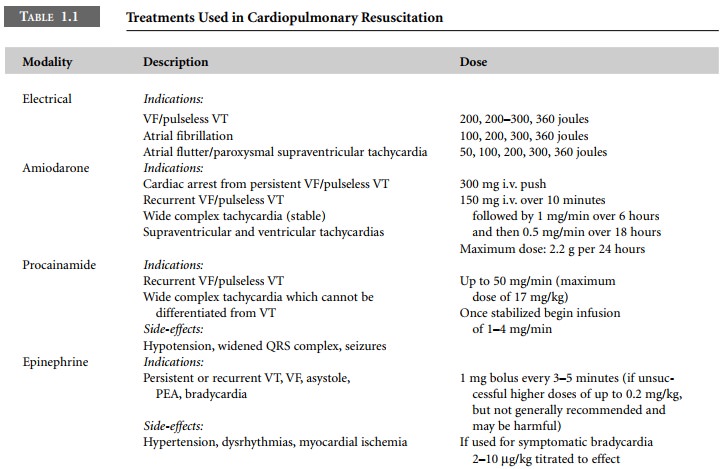
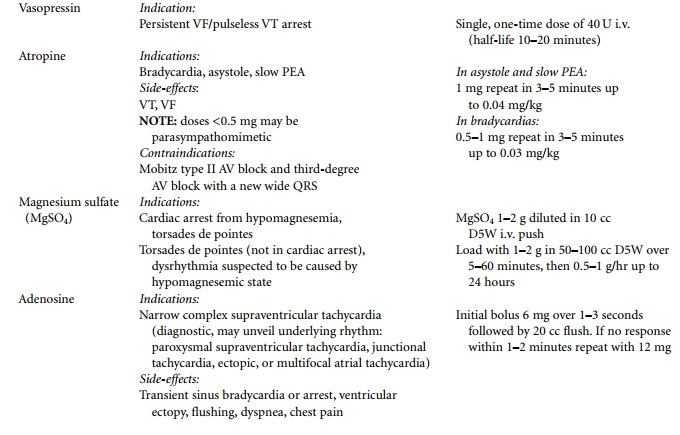
patient with impaired ventricular function (Table 1.1).

Related Topics