Chapter: Clinical Cases in Anesthesia : Congestive Heart Failure
What is the pathophysiology of dilated cardiomyopathy?
What is
the pathophysiology of dilated cardiomy-opathy?
The dilated cardiomyopathies are characterized
by elevated filling pressures, failure of myocardial contractile strength, and
a marked inverse relationship between arterial impedance and stroke volume. The
dilated cardio-myopathies present a picture very similar to that of CHF
produced by severe coronary artery disease (CAD).
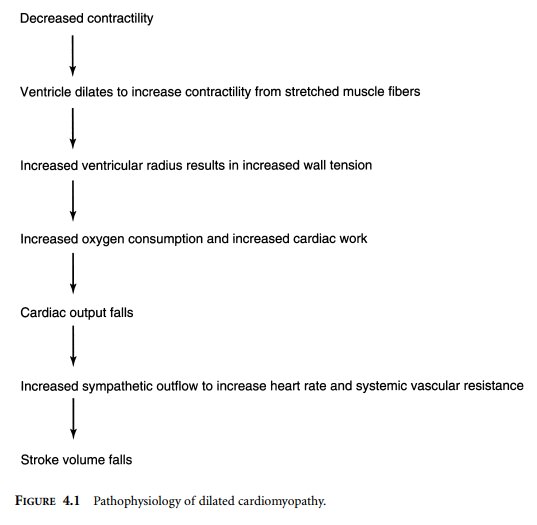
The pathophysiologic considerations are familiar ones. As the ventricular muscle weakens, the ventricle dilates in order to take advantage of the increased force of contraction resulting from increasing myocardial fiber length. As the ventricular radius increases, however, ventricular wall tension rises, increasing both the oxygen consumption of the myocardium and the total internal work of the muscle. As the myocardium deteriorates further, the cardiac output falls, and a compensatory increase in sympathetic activity occurs to maintain organ perfusion and cardiac output.
One feature of the failing myocardium is the
loss of its ability to maintain stroke volume in the face of increased arterial
impedance to ejection. As left ventricular dysfunc-tion worsens, stroke volume
becomes more dependent on arterial impedance (afterload). In the failing
ventricle, stroke volume falls almost linearly with increases in afterload. The
increased sympathetic outflow that accom-panies left ventricular failure
initiates a vicious cycle of increased resistance to forward flow, decreased
stroke volume and cardiac output, and further sympathetic stimu-lation in an
effort to maintain circulatory homeostasis (Figure 4.1).
There is some degree of mitral regurgitation in
severe dilated cardiomyopathies due to stretching of the mitral annulus and
distortion of the geometry of the chordae tendineae. The forward stroke volume
improves with after-load reduction, even though there is no increase in
ejection fraction. This suggests that reduction of mitral regurgitation is the
mechanism of the improvement. Afterload reduction also decreases left
ventricular filling pressure, which relieves
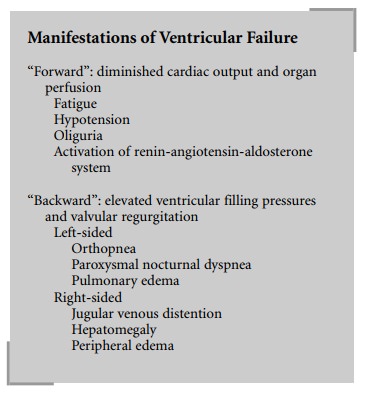
The clinical picture of the dilated
cardiomyopathies falls into the two familiar categories of “forward” failure
and “backward” failure. The features of “forward” failure, such as fatigue,
hypotension, and oliguria, are due to diminished cardiac output and organ
perfusion. Decreased renal perfusion results in activation of the
renin-angiotensin-aldosterone system that increases the effective circulating
blood volume through sodium and water retention. “Backward” failure is related
to the elevated filling pressures required by the failing ventricle(s). As the
left ventricle dilates, “secondary” mitral regurgitation occurs due to the
mechanisms noted above. The manifestations of left-sided ventricular failure
include orthopnea, paroxysmal nocturnal dyspnea, and pulmonary edema. The
manifestations of right-sided ventricular failure include hepatomegaly, jugular
venous distention, and peripheral edema.
Related Topics