Chapter: Clinical Cases in Anesthesia : Cardiopulmonary Resuscitation
What is the antidysrhythmic therapy of choice in VF/pulseless VT?
What is
the antidysrhythmic therapy of choice in VF/pulseless VT?
After CPR has been initiated and the underlying
rhythm recognized, immediate defibrillation is the mainstay therapy in the
treatment of VF/pulseless VT. The choice of antidys-rhythmic therapy has not
been shown to influence outcome if repeated countershocks,
epinephrine/vasopressin, and appropriately administered CPR are ineffective in
a patient with refractory VF or VT. No drug has clearly proven supe-riority in
most cases of intractable VT or VF. Despite this, the 2000 ACLS protocol
contains many changes in drug administration in VF/pulseless VT compared with
older recommendations. Lidocaine is no longer recommended as the
antidysrhythmic drug of choice for the treatment of malignant ventricular
ectopy, VT, or VF. Lidocaine and procainamide hydrochloride are now classified
as drugs with intermediate evidence for this indication. Bretylium is no longer
recommended and has been removed from the ACLS algorithm. Instead, amiodarone
is now a Class IIb indication for cardiac arrest from VF/pulseless VT that
persists after multiple shocks. Amiodarone has been shown to increase the
intermediate outcome of admission-to-hospital following out-of-hospital
refractory VF arrest in one prospective double-blinded randomized controlled
study.
Nonetheless, amiodarone administration is not
associated with improvement of long-term outcome. After attempts to
defibrillate and epinephrine and/or vasopressin adminis-tration fail to
establish a perfusing rhythm, the new ACLS guidelines indicate consideration of
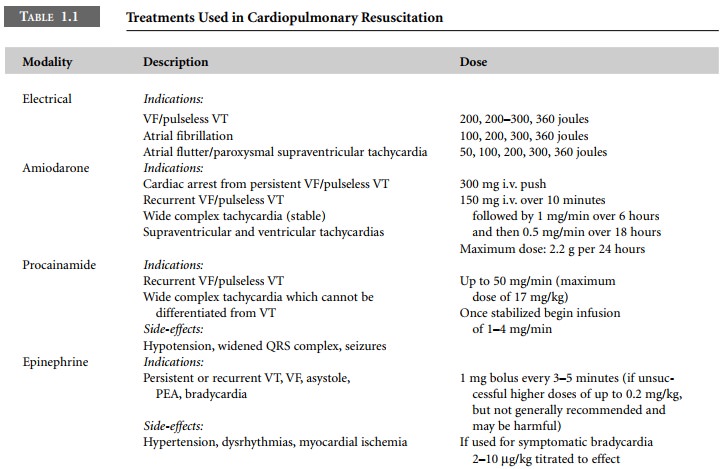
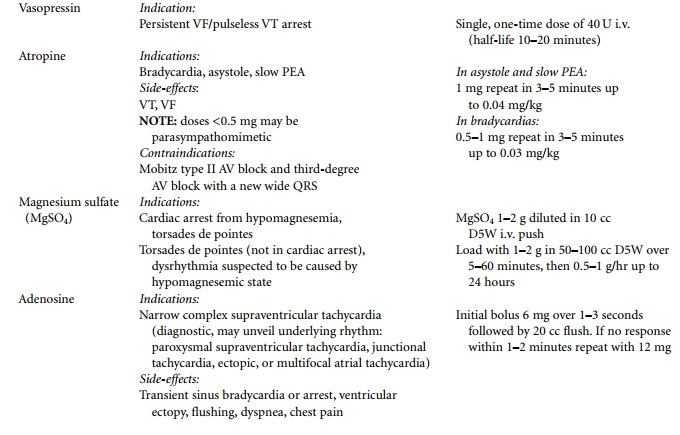
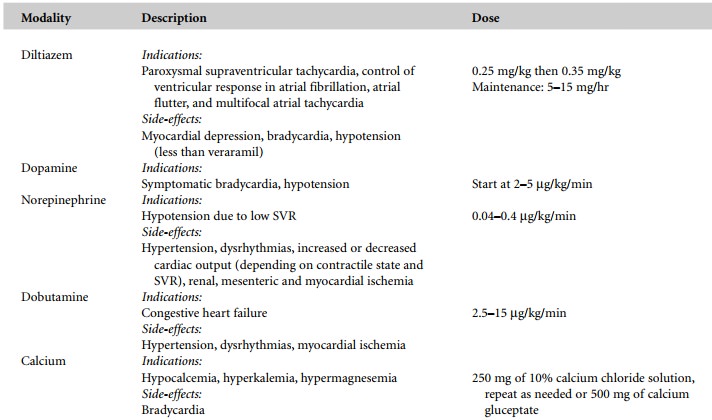
antidysrhythmics as follows (Table 1.1):

·
amiodarone
300 mg i.v. push for persistent or recurrent VF/pulseless VT
·
magnesium
sulfate 1–2 mg i.v. when an underlying hypo-magnesemic state is suspected or in
torsades de pointes
·
procainamide
50 mg/min in refractory VF (maximum 17 mg/kg)
Related Topics