Chapter: Clinical Cases in Anesthesia : Recent Myocardial Infarction
What intraoperative monitors would you use?
What intraoperative monitors would you use?
A general goal in these patients is to maintain
intraoperative hemodynamics within 20% of preoperative values. Therefore, in
addition to the standard intraoperative monitors, other monitors that should be
considered include an intra-arterial line, a pulmonary artery catheter (PAC),
and a TEE. An intra-arterial line would be the optimum way of monitoring blood
pressure (BP) beat-to-beat. Although 40% of intraoperative ischemic episodes
are not related to aberrations in hemodynamics, there are studies demonstrating
that inadequate management of hemody-namic abnormalities may increase risk.
Hypotension (BP <30% baseline for greater than 10 minutes) has been shown to
be a strong predictor of PCE in one study. On the other hand, there are no
studies demonstrating conclusively that hypertension is associated with adverse
outcome. Tachycardia has not been definitely shown to be associated with PCE,
although studies suggest a relationship.
The easiest technique for myocardial ischemia
monitoring in the anesthetized patient is with a multiple-lead ECG. Monitoring
precordial chest leads V4 and V5 detects greater than 90%
of ischemic events that would be seen on a 12-lead ECG, but it has been
reported to have as low as a 9% sensitivity compared with the gold standard
(myo-cardial lactate extraction). ST-segment depressions and T-wave morphology
changes are most commonly seen. However, there are patients in whom the ECG is
not an effective intraoperative monitor of myocardial ischemia, such as those
with LV hypertrophy, conduction abnormal-ities, and ventricular pacemaker
dependence.
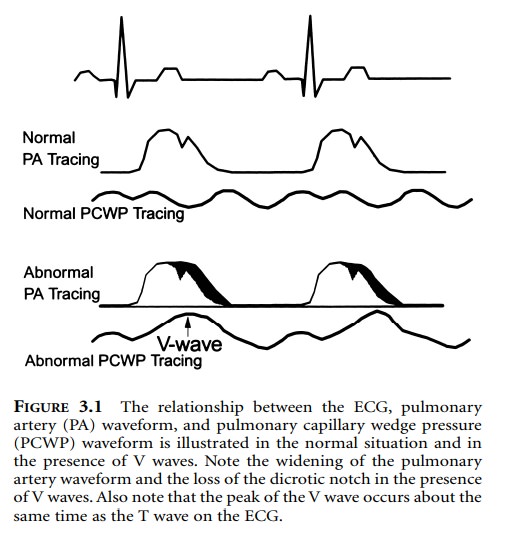
The development of V waves on the pulmonary
artery wedge pressure waveform may be an indication of myocar-dial ischemia,
but it is not sensitive or specific enough to be regarded as a reliable monitor
for this purpose (Figure 3.1).
The utility of the PAC, however, extends beyond
its ques-tionable ability to detect ischemia. It provides information about the
patient’s intravascular volume status, a quantitative estimate of myocardial
compliance, and allows for calcula-tion of cardiac output and other hemodynamic
measure-ments, such as systemic vascular resistance and stroke volume. A PAC
would be mandatory if this patient showed signs of CHF preoperatively.
The TEE is the most sensitive detector of
intraoperative ischemia, and it is capable of detecting ischemia earlier than
any other modality. However, studies have questioned its specificity.
Specifically, it is not clear what TEE changes are predictive of ischemia and
PCE. In the largest study of patients with or at-risk for CAD who were
scheduled for noncardiac surgery, Mangano and Goldman (1995) did not find that
LV wall motion abnormalities were predictive of ischemia or PCE. The TEE also
provides physiologic information, such as estimates of LV ejection fraction and
intravascular volume status, which may help with intraoperative management in
patients with ventricular dysfunction.
Related Topics