Chapter: Clinical Cases in Anesthesia : Coronary Artery Disease
What are the determinants of myocardial oxygen consumption (demand)?
What are
the determinants of myocardial oxygen consumption (demand)?
Heart rate, contractility, and myocardial wall
tension are the three major determinants of myocardial oxygen
Heart rate is probably the most
important parameter regulating the myocardial oxygen supply-demand balance.
Decreasing heart rate both increases oxygen supply by prolonging diastole and
decreases oxygen demand. The association between tachycardia and myocardial
ischemia is well documented. Severe bradycardia should be avoided, however, as
this will cause decreased diastolic arterial pres-sure and increased left
ventricular end-diastolic pressure. β-Adrenergic blocking drugs are commonly used to
main-tain a mild bradycardia in patients with CAD.
Myocardial contractility is loosely defined as
the intrinsic ability of the myocardium to shorten. This is a very difficult
parameter to measure and is poorly described by the cardiac output or even the
left ventricular ejection fraction. Decreased myocardial contractility is
associated with decreased myocardial oxygen demand. Thus, “myocardial
depression” may be beneficial in patients with CAD. Specifically, agents that
depress myocardial contractility but are not potent vasodilators may be
beneficial as long as coronary perfusion pressure is maintained. Thus, potent
volatile anesthetic agents (halothane, enflurane, and isoflu-rane) are examples
of “myocardial depressants” that could be useful for patients with CAD as long
as coronary perfusion pressure is maintained.
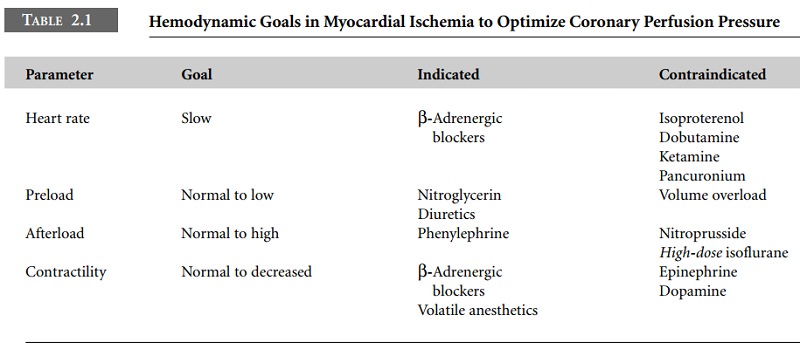
Myocardial oxygen supply and demand are kept in
balance by properly managing left ventricular preload, afterload, heart rate,
and contractility. Major increases in preload (left ventricular end-diastolic
volume) add to the volume work of the heart (increased demand) and decrease
coronary perfusion pressure because of the asso-ciated increase in left
ventricular end-diastolic pressure (decreased supply). Nitrates assist in
maintaining a normal to low preload (see below). Excessive increases in
afterload result in increased pressure work of the heart (wall tension) during
systole (increased demand) despite the increase in coronary perfusion pressure.
At the other end of the spectrum, extreme vasodilatation (decreased afterload)
will lower the diastolic arterial pressure and decrease myocardial oxygen
supply (see Table 2.1).
Related Topics