Chapter: Clinical Cases in Anesthesia : Eisenmenger Syndrome (Subacute Bacterial Endocarditis Prophylaxis)
What are the anesthetic considerations for a patient with Eisenmenger syndrome?
What are
the anesthetic considerations for a patient with Eisenmenger syndrome?
Eisenmenger syndrome occurs in patients with
congenital heart disease (CHD) who have had prolonged shunting of blood to the
lungs with excessive pulmonary blood flow and pressure. It occurs after several
years in patients who have uncorrected cardiac lesions, such as atrial septal
defects, ventricular septal defects, or patent ductus arteriosus, with pulmonary-to-systemic
blood flow ratios greater than 2:1 (left-to-right shunting). As irreversible
changes occur in the pulmonary vasculature, the pulmonary vascular resistance
(PVR) rises to the point where there is reversal of flow across the cardiac
defect resulting in cyanosis (right-to-left shunting).
Once right-to-left shunting occurs, the cardiac
defect is no longer surgically correctable. In Eisenmenger syndrome, the PVR is
so high that an attempted surgical closure of the defect would cause the right
ventricle to fail due to the increased impedance to ejection. The only possible
surgi-cal treatment is heart-lung transplantation. Untreated Eisenmenger
syndrome is associated with a poor long-term prognosis. These patients are at
greatly increased risk for any elective procedure. They are usually
anesthetized for emergency procedures as well as labor and delivery.
The anesthetic considerations are similar to
those in any patient with CHD and right-to-left shunting. These con-cerns
include managing a patient who could decompensate due to increased
right-to-left shunting with worsened hypoxemia and/or myocardial dysfunction.
Polycythemia is a major preoperative concern in these patients who are at risk
of having thrombotic complications, especially if they are dehydrated.
Preoperative phlebotomy or autologous blood donation should be considered if
the hematocrit is >55–60%. These patients are also at high risk of
paradoxi-cal embolization and bacterial endocarditis.
The ratio of pulmonary-to-systemic blood flow depends
on the ratio of PVR to systemic vascular resistance (SVR). A decrease in SVR or
an increase in PVR will increase right-to-left shunting and increase cyanosis.
PVR is increased with low inspired oxygen concentration, acidosis, hypercarbia,
hypothermia, high lung inflation pressures or positive end-expiratory
pressures, endobronchial intubation, and high catecholamine levels.
The goal is to maintain the baseline PVR:SVR
ratio. Preoperatively, the patient should be well hydrated. These patients may
receive anesthetic premedication, but do not tolerate respiratory depression
well. Supplemental oxygen may be helpful following sedative medications.
Monitoring should be tailored to the procedure, but an intra-arterial line is
indicated in all but the most minor procedures, such as monitored cases
performed under local anesthesia. The indications for a pulmonary artery
catheter are controversial. It may be impossible to enter the pulmonary artery,
and the placement and maintenance of the pulmonary artery catheter may result
in significant morbidity and mortality. A central line can often serve as an
indicator of right ventricular function and allows for central administration
of medications.
The anesthetic should be designed to minimize
myocar-dial depression and PVR. To avoid enlarging any inadvertent air emboli,
it is probably wisest to avoid nitrous oxide. Regional and general anesthetics
have been used successfully but require judicious management, invasive
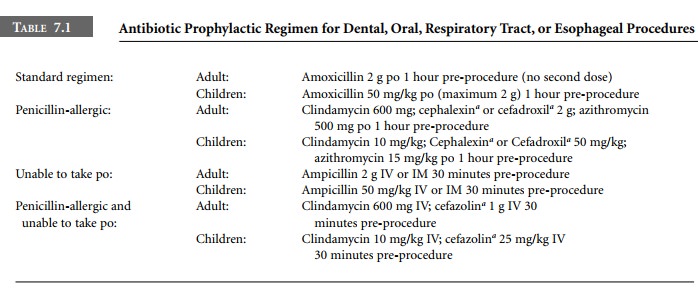
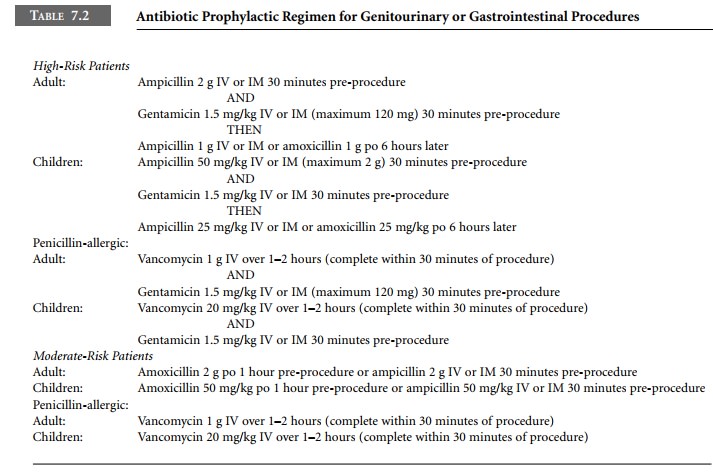
monitoring, and appropriate hemodynamic interventions. For prophy-laxis against
endocarditis, antibiotics must be administered early enough so that therapeutic
tissue levels are achieved at the time of skin incision, and postoperative
doses must be ordered (Tables 7.1, 7.2). Arrangements should be made to closely
monitor the patient postoperatively.
Related Topics