Chapter: Psychiatric Mental Health Nursing : Client’s Response to Illness
Individual Factors - Client’s Response to Illness
INDIVIDUAL FACTORS
Age, Growth, and Development
A person’s age seems to affect how he or she copes with illness.
For instance, the age at onset of schizophrenia is a strong predictor of the
prognosis of the disease (Buchanan & Carpenter, 2005). People with a
younger age at onset have poorer outcomes, such as more negative signs (apathy,
social isolation, and lack of volition) and less effective coping skills, than
do people with a later age at onset. A possible reason for this difference is
that younger clients have not had experi-ences of successful independent living
or the opportunity to work and be self-sufficient and have a less
well-developed sense of personal identity than older clients.
A client’s age also can influence how he or she expresses illness.
A young child with attention deficit hyperactivity disorder may lack the
understanding and ability to describe his or her feelings, which may make
management of the disorder more challenging. Nurses must be aware of the
child’s level of language and work to understand the expe-rience as he or she
describes it.
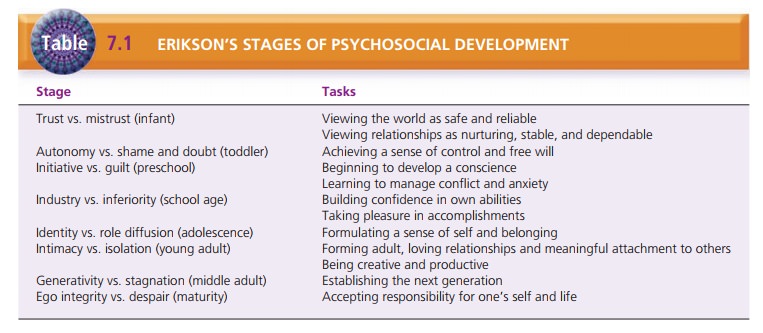
Erik Erikson described psychosocial development across the life
span in terms of developmental tasks to accomplish at each stage (Table 7.1).
Each stage of development depends on the successful completion of the previous
stage. In eachstage, the person must complete a critical life task that is
essential to well-being and mental health. Failure to com-plete the critical
task results in a negative outcome for that stage of development and impedes
completion of future tasks. For example, the infancy stage (birth to 18 months)
is the stage of “trust versus mistrust,” when infants must learn to develop
basic trust that their parents or guardians will take care of them, feed them,
change their diapers, love them, and keep them safe. If the infant does not develop
trust in this stage, he or she may be unable to love and trust others later in
life because the ability to trust others is essential to establishing good
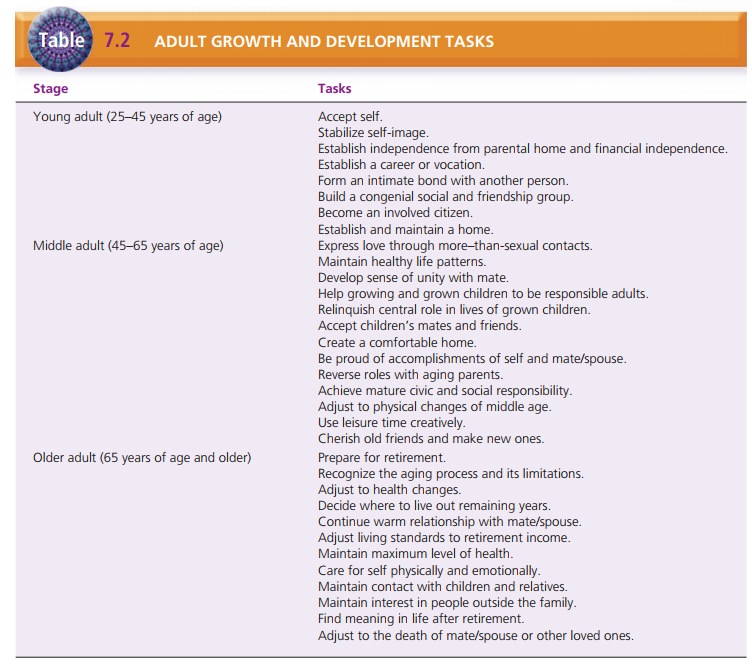
relationships. Specific devel-opmental tasks for adults are summarized in Table
7.2.
![]()
![]()
According to Erikson’s theory, people may get “stuck” at any stage
of development. For example, a person who never completed the developmental
task of autonomy may become overly dependent on others. Failure to develop
identity can result in role confusion or an unclear idea about whom one is as a
person. Negotiating these develop-mental tasks affects how the person responds
to stress and illness. Lack of success may result in feelings of inferiority,
doubt, lack of confidence, and isolation—all of which can affect how a person
responds to illness.
Genetics and Biologic Factors
Heredity and biologic factors are not under voluntary con-trol. We
cannot change these factors. Research has identi-fied genetic links to several
disorders. For example, some people are born with a gene associated with one
type of Alzheimer’s disease. Although specific genetic links have not been
identified for several mental disorders (e.g., bipo-lar disorder, major depression,
and alcoholism), research has shown that these disorders tend to appear more
fre-quently in families. Genetic makeup tremendously influ-ences a person’s
response to illness and perhaps even totreatment. Hence, family history and
background are essential parts of the nursing assessment.
Physical Health and Health Practices
Physical health also can influence how a person responds to
psychosocial stress or illness. The healthier a person is, the better he or she
can cope with stress or illness. Poor nutri-tional status, lack of sleep, or a
chronic physical illness may impair a person’s ability to cope. Unlike genetic
factors, how a person lives and takes care of himself or herself can alter many
of these factors. For this reason, nurses must assess the client’s physical
health even when the client is seeking help for mental health problems.
Personal health practices, such as exercise, can influence the
client’s response to illness. Exercising is one self-help inter-vention that
can diminish the negative effects of depressionand anxiety (Morgan & Jorm,
2008). Further, when individu-als participated with others in exercise, the
members of the group reported increased social support and an improved sense of
well-being (Carless & Douglas, 2008). This suggests that continued
participation in exercise is a positive indicator of improved health, whereas
cessation from participation in exer-cise might indicate declining mental
health.
Response to Drugs
Biologic differences can affect a client’s response to treat-ment,
specifically to psychotropic drugs. Ethnic groups differ in the metabolism and
efficacy of psychoactive com-pounds. Some ethnic groups metabolize drugs more
slowly (meaning the serum level of the drug remains higher), which increases
the frequency and severity of side effects. Clients who metabolize drugs more
slowly generally need lower doses of a drug to produce the desired effect
(Purnell
·
Paulanka, 2008). In general, nonwhites treated with Western dosing
protocols have higher serum levels per dose and suffer more side effects.
Although many non-Western countries report successful treatment with lower
dosages of psychotropic drugs, Western dosage protocols continue to drive
prescribing practices in the United States. When evaluating the efficacy of psychotropic
medications, the nurse must be alert to side effects and serum drug lev-els in
clients from different ethnic backgrounds.
Self-Efficacy
Self-efficacy is a belief that personal
abilities and efforts affect the
events in our lives. A person who believes that his or her behavior makes a
difference is more likely to take action. People with high self-efficacy set
personal goals, are self-motivated, cope effectively with stress, and request
support from others when needed. People with low self-efficacy have low
aspirations, experience much self-doubt, and may be plagued by anxiety and
depression. It has been suggested that focusing treatment on developing a
client’s skills to take control of his or her life (developing self-effi-cacy)
so that he or she can make life changes could be very beneficial. Four main
ways to do so follow:
a. Experience of success or
mastery in overcoming obstacles
b.
Social modeling (observing successful people instills the idea that
one can also succeed)
c. Social persuasion (persuading
people to believe in themselves)
d. Reducing stress, building
physical strength, and learning how to interpret physical sensations positively
(e.g., view-ing fatigue as a sign that one has accomplished some-thing rather
than as a lack of stamina).
![]()
![]()
Cutler (2005) reports a relationship between self-efficacy and the
client’s motivation for self-care and follow-up after discharge from treatment.
Clients returning to the commu-nity with higher self-efficacy were more
confident and had positive expectations about their personal success. Cutler
suggests that therapeutic interventions designed to promote the client’s
self-efficacy can have positive effects on interper-sonal relationships and
coping on return to the community.
Hardiness
Hardiness is the ability to resist
illness when under stress. First
described by Kobasa (1979), hardiness has three components:
·
Commitment: active involvement in life
activities
·
Control: ability to make appropriate
decisions in life activities
·
Challenge: ability to perceive change
as beneficial rather than just
stressful.
Hardiness has been found to have a moderating or buffer-ing effect
on people experiencing stress. Kobasa (1979) found that male executives who had
high stress but low occurrence of illness scored higher on the hardiness scale
than executives with high stress and high occurrence of illness. Study findings
suggested that stressful life events caused more harm to people with low
hardiness than with high hardiness.
Personal hardiness is often described as a pattern of atti-tudes
and actions that helps the person turn stressful cir-cumstances into
opportunities for growth. Maddi (2005) found that persons with high hardiness
perceived stressors more accurately and were able to problem-solve in the
situa-tion more effectively. Hardiness has been identified as an important
resilience factor for families coping with the mental illness of one of their
members (Greeff, Vansteenween, & Mieke, 2006).
Some believe that the concept of hardiness is vague and indistinct and
may not help everyone. Some research on hardiness suggests that its effects are
not the same for men and women. In addition, hardiness may be useful only to
those who value individualism, such as people from some Western cultures. For
people and cultures who value rela-tionships over individual achievement,
hardiness may not be beneficial.
Resilience and Resourcefulness
Two closely related concepts, resilience and resourceful-ness, help
people to cope with stress and to minimize the![]()
![]() effects of illness (Edward & Warelow,
2005). Resilience is defined as
having healthy responses to stressful circum-stances or risky situations. This
concept helps to explain why one person reacts to a slightly stressful event
with severe anxiety, whereas another person does not experi-ence distress even
when confronting a major disruption.
effects of illness (Edward & Warelow,
2005). Resilience is defined as
having healthy responses to stressful circum-stances or risky situations. This
concept helps to explain why one person reacts to a slightly stressful event
with severe anxiety, whereas another person does not experi-ence distress even
when confronting a major disruption.
Keyes (2007) found that high resilience was associated with
promoting and protecting one’s mental health, described as flourishing. Family
resilience refers to the successful cop-ing of family members under stress
(Black & Lobo, 2008). Factors that are present in resilient families
include positive outlook, spirituality, family member accord, flexibility,
fam-ily communication, and support networks. Resilient families also spend time
together, share recreational activities, and participate in family rituals and
routines together.
Resourcefulness involves using
problem-solving abili-ties and believing that one can cope with adverse or
novel situations. People develop resourcefulness through inter-actions with
others, that is, through successfully coping with life experiences. Examples of
resourcefulness include performing health-seeking behaviors, learning
self-care, monitoring one’s thoughts and feelings about stressful sit-uations,
and taking action to deal with stressful circum-stances. Chang, Zauszniewski,
Heinzer, Musil, and Tsai (2007) found building resourcefulness skills to be the
key in reducing depressive symptoms and enhancing adaptive functioning among
middle school children whose female caregivers were depressed.
Spirituality
Spirituality involves the essence of a
person’s being and his or her
beliefs about the meaning of life and the purpose for living. It may include
belief in God or a higher power, the practice of religion, cultural beliefs and
practices, and a relationship with the environment. Although many clients with
mental disorders have disturbing religious delusions, for many in the general
population, religion and spiritual-ity are a source of comfort and help in times
of stress or trauma. Studies have shown that spirituality is a genuine help to
many adults with mental illness, serving as a pri-mary coping device and a
source of meaning and coher-ence in their lives or helping to provide a social
network (Anthony, 2008).
Religious activities, such as church attendance and praying, and
associated social support have been shown to be very important for many people
and are linked with better health and a sense of well-being. These activities
also have been found to help people cope with poor health. Hope and faith have
been identified as critical factors in psychiatric and physical rehabilitation.
Chaudry (2008) described patients who depended on their religious faith as
significantly less depressed and anxious than those who are less reliant on
their faith. Religion and spirituality can also be helpful to families who have
a relative with mental illness, providing support and solace to caregivers.
Becausespiritual or religious beliefs and practices help many clients to cope
with stress and illness, the nurse must be particu-larly sensitive to and
accepting of such beliefs and prac-tices. Incorporating those practices into
the care of clients can help them cope with illness and find meaning and
pur-pose in the situation. Doing so can also offer a strong source of support
(Huguelet, Mohr, Borras, Gillieron, & Brandt, 2006).
Related Topics