Chapter: Clinical Cases in Anesthesia : Congestive Heart Failure
How would you anesthetize this patient?
How would you anesthetize this patient?
The avoidance of myocardial depression still
remains the goal of anesthetic management for patients with dilated
cardiomyopathy. All the potent volatile anesthetic agents are myocardial
depressants. For this reason, these agents, especially in high concentrations,
are probably best avoided in this group of patients. An anesthetic based on a
combination of narcotics and sedative-hypnotics (with or without nitrous oxide)
can be employed instead. Etomidate and ketamine are acceptable anesthetic
induction agents, while thiopental and propofol are relatively contraindicated.
For the patient with a severely compromised
myo-cardium, the synthetic piperidine opioids (fentanyl, sufen-tanil,
remifentanil, and alfentanil) are useful, since myocardial contractility is not
depressed. Chest wall rigidity associated with these medications is treated
with muscle relaxants. Bradycardia associated with high-dose opioid anesthesia
may be prevented by the use of pancuronium for muscle relaxation,
anticholinergic drugs, or pacing. For peripheral or lower abdominal surgical
procedures, the use of a regional anesthetic technique is a reasonable
alternative, provided filling pressures are carefully controlled and the
hemodynamic effects of the anesthetic are adequately monitored. Regional
techniques may not be possible in many patients due to anticoagulation for
associated atrial fibrillation or mural thrombus prevention.
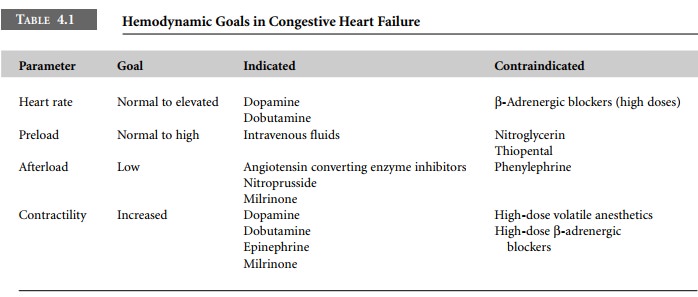
In planning the anesthetic management of the
patient with dilated cardiomyopathy, associated cardiovascular conditions, such
as the presence of CAD, valvular abnormal-ities, outflow tract obstruction, and
constrictive pericarditis, should also be considered. Patients with CHF often
require circulatory support intra- and postoperatively. Inotropic drugs, such
as dopamine or dobutamine, have been shown to be effective in low-output
states, and produce modest changes in systemic vascular resistance at lower
dosages. In severe failure, more potent drugs, such as epinephrine, may be
required. The effects of β-adrenergic agents are limited, however, by the
downregulation of β-adrenergic receptors that occurs in chronic
CHF. Milrinone is a phosphodiesterase inhibitor with inotropic and vasodilator
properties that may improve hemodynamic performance. As noted above, stroke
volume is inversely related to afterload in the failing ventricle, and reducing
left ventricular afterload with vasodilating drugs, such as nitroprusside and
milrinone, is also effective in increasing cardiac output. In patients with
myocarditis, especially of the viral variety, transvenous or external pacing
may be required should heart block occur. Intra-aortic balloon counterpulsation
and left ventricular assist devices are further options to be considered in the
case of the severely compromised ventricle.
There is a definite increase in the incidence
of supra-ventricular and ventricular dysrhythmias in myocarditis and the
dilated cardiomyopathies. These dysrhythmias often require extensive
electrophysiologic investigation, and may be unresponsive to maximal medical
therapy.
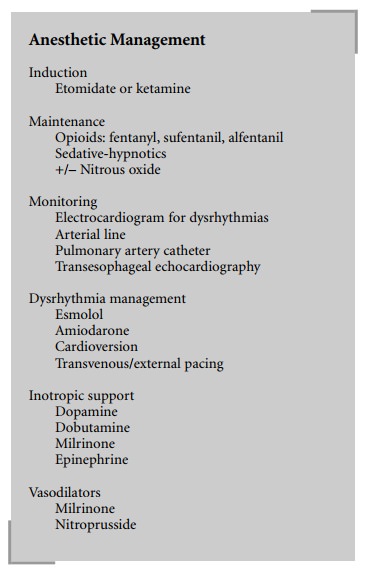
Anesthetic
Management
Induction
Etomidate or ketamine
Maintenance
Opioids: fentanyl, sufentanil, alfentanil
Sedative-hypnotics
+/– Nitrous oxide
Monitoring
Electrocardiogram
for dysrhythmias Arterial line
Pulmonary
artery catheter Transesophageal echocardiography
Dysrhythmia management
Esmolol
Amiodarone
Cardioversion
Transvenous/external pacing
Inotropic support
Dopamine
Dobutamine
Milrinone
Epinephrine
Vasodilators
Milrinone
Nitroprusside
Implantable cardioverter-defibrillators are
often implanted in these patients, and must be turned off during surgery
requiring electrocautery. Thus, proper ECG monitoring and access to a charged
external cardioversion device are crucial in the management of these patients.
Amiodarone is a long-acting antidysrhythmic medication with intrinsic
myocardial depressant properties. Nevertheless, amio-darone seems to have an
overall beneficial effect in patients with CHF, especially those who present
with chronic atrial fibrillation. Furthermore, amiodarone is currently the
antiarrhythmic medication of choice in persistent ventricu-lar
tachycardia/ventricular fibrillation, which may be encountered at any time in
patients with severely impaired myocardial function (Table 4.1)
Related Topics