Chapter: Clinical Cases in Anesthesia : The Jehovah’s Witness Patient
Describe the intraoperative anesthetic considerations for posterior spinal fusion surgery
Describe the intraoperative anesthetic considerations for posterior
spinal fusion surgery.
An inhalation or intravenous induction is
acceptable. Any of the nondepolarizing muscle relaxants can be used for this
procedure. A balanced technique of nitrous oxide, oxygen, volatile agent,
neuromuscular blocker, and an opioid should be considered for the maintenance
anesthetic. If somatosensory and/or motor evoked potential monitoring are to be
used, then it is recommended that the concentration of the volatile agent be
0.2% or less. An opioid infusion rather than bolus injections is the preferred
anesthetic technique, particularly in the presence of evoked potential
monitoring.
In addition to the standard intraoperative
monitors, an arterial catheter, central venous catheter, and a urinary catheter
should be placed. The arterial catheter allows for monitoring of arterial blood
pressure on a beat-to-beat basis and also facilitates blood sampling. Most
anesthesiol-ogists will opt for placement of a central venous catheter to
monitor central filling pressures and volume status. Depending on the severity
of cardiopulmonary disease, a pulmonary artery catheter may be warranted.
Turning and positioning the patient prone
requires extreme care. It is important to avoid pressure on the eyes, which can
result in retinal artery occlusion and blindness. It is also necessary to avoid
pressure necrosis of the ears, nose, and forehead. The head should be in proper
align-ment and positioned in such a way that allows for easy inspection of the
face. The chest, abdomen, and pelvic areas should rest on properly positioned
parallel rolls or other devices that avoid pressure on the axilla, breasts and
genitalia. The arms should rest at the sides with the elbows flexed and the
shoulders abducted no greater than 90° to avoid stretching the brachial plexus.
Appropriate padding should also be present.
A considerable decrease in body temperature can
occur during spinal surgery on account of the large body surface area exposed.
Precautions should be taken to avoid intra-operative hypothermia. These include
using a forced-air warming blanket, an intravenous fluid warming system, and
adjustment of the operating room temperature.
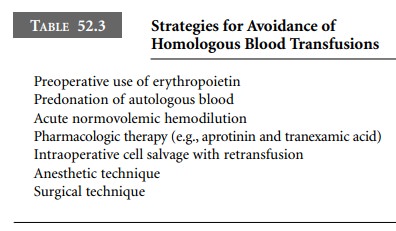
Significant blood loss is not uncommon during
this surgery. Predonation of autologous blood is efficacious and recommended
for spinal fusion surgery. There are several techniques designed to minimize
blood loss and the need for homologous blood transfusion (Table 52.3). More
specifically, the intraoperative techniques are acute normo-volemic
hemodilution, cell salvage, hypotensive anesthesia, surgical technique, and
local infiltration with an epineph-rine-containing solution. The latter
technique helps to reduce bleeding at the site of infiltration, but the overall
reduction in surgical blood loss is minimal.
A review of each hypotensive anesthetic
technique (Table 52.4) is beyond the scope of this chapter. There are a number
of excellent resources available for review of these techniques. However, there
are several key points to keep in mind when using hypotensive anesthesia. The
mean arterial pressure (MAP) should be maintained above 50 mmHg to ensure
adequate spinal cord perfusion and cerebral blood flow. In general, a MAP of
50–60 mmHg is ideal. In addition, the arterial blood gases should be monitored
during the procedure.
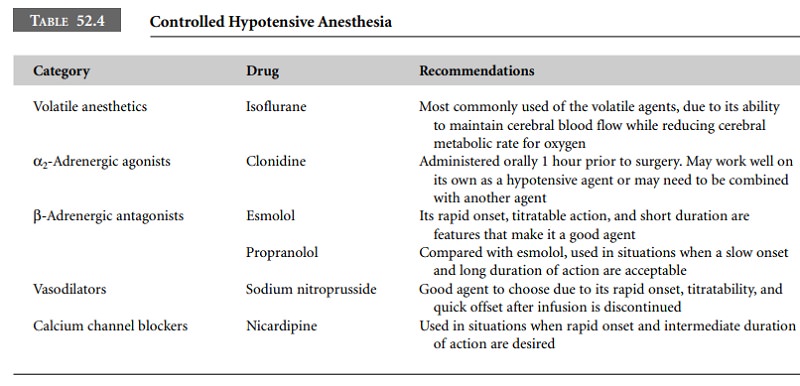
Contraindications to the use of controlled
hypotension include pre-existing major end-organ dysfunction,
hemo-globinopathies, polycythemia, and elevated intracranial pressure. The
clinician must have a thorough understanding of the technique and also be
competent with the use of the technique chosen.
Related Topics