Chapter: Basic & Clinical Pharmacology : Agents Used in Cardiac Arrhythmias
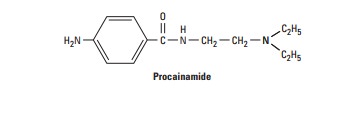
Procainamide (Subgroup 1A)
SODIUM CHANNEL-BLOCKING DRUGS (CLASS 1)
Drugs with local anesthetic action block sodium channels and reduce the sodium current, INa. They are the oldest group of anti-arrhythmic drugs and are still widely used.
PROCAINAMIDE (SUBGROUP 1A)
Cardiac Effects
By blocking sodium channels, procainamide slows the upstroke of the action potential, slows conduction, and prolongs the QRS duration of the ECG. The drug also prolongs the APD (a class 3 action) by nonspecific blockade of potassium channels. The drug may be somewhat less effective than quinidine in suppressing abnormal ectopic pacemaker activity but more effec-tive in blocking sodium channels in depolarized cells.
Procainamide has direct depressant actions on SA and AV nodes, and these actions are only slightly counterbalanced by drug-induced vagal block.
Extracardiac Effects
Procainamide has ganglion-blocking properties. This action reduces peripheral vascular resistance and can cause hypotension, particularly with intravenous use. However, in therapeutic concentrations, its peripheral vascular effects are less prominent than those of quinidine. Hypotension is usually associated with excessively rapid procainamide infusion or the presence of severe underlying left ventricular dysfunction.
Toxicity
Procainamide’s cardiotoxic effects include excessive action potential prolongation, QT-interval prolongation, and induction of torsades de pointes arrhythmia and syncope. Excessive slowing of conduction can also occur. New arrhythmias can be precipitated.
troublesome adverse effect of long-term procainamide therapy is a syndrome resembling lupus erythematosus and usu-ally consisting of arthralgia and arthritis. In some patients, pleuritis, pericarditis, or parenchymal pulmonary disease also occurs. Renal lupus is rarely induced by procainamide. During long-term therapy, serologic abnormalities (eg, increased anti-nuclear antibody titer) occur in nearly all patients, and in the absence of symptoms, these are not an indication to stop drug therapy. Approximately one third of patients receiving long-term procainamide therapy develop these reversible lupus-related symptoms.
Other adverse effects include nausea and diarrhea (in about 10% of cases), rash, fever, hepatitis (< 5%), and agranulocytosis (approximately 0.2%).
Pharmacokinetics & Dosage
Procainamide can be administered safely by intravenous and intra-muscular routes and is well absorbed orally. A metabolite (N-acetylprocainamide, NAPA) has class 3 activity. Excessive accumulation of NAPA has been implicated in torsades de pointes during procainamide therapy, especially in patients with renal failure. Some individuals rapidly acetylate procainamide and develop high levels of NAPA. The lupus syndrome appears to be less common in these patients.
Procainamide is eliminated by hepatic metabolism to NAPA and by renal elimination. Its half-life is only 3–4 hours, which necessitates frequent dosing or use of a slow-release formulation (the usual practice). NAPA is eliminated by the kidneys. Thus, procainamide dosage must be reduced in patients with renal fail-ure. The reduced volume of distribution and renal clearance associ-ated with heart failure also require reduction in dosage. The half-life of NAPA is considerably longer than that of procainamide, and it therefore accumulates more slowly. Thus, it is important to measure plasma levels of both procainamide and NAPA, especially in patients with circulatory or renal impairment.
If a rapid procainamide effect is needed, an intravenous load-ing dose of up to 12 mg/kg can be given at a rate of 0.3 mg/kg/ min or less rapidly. This dose is followed by a maintenance dosage of 2–5 mg/min, with careful monitoring of plasma levels. The riskof gastrointestinal (GI) or cardiac toxicity rises at plasma concen-trations greater than 8 mcg/mL or NAPA concentrations greater than 20 mcg/mL.
To control ventricular arrhythmias, a total procainamide dos-age of 2–5 g/d is usually required. In an occasional patient who accumulates high levels of NAPA, less frequent dosing may be possible. This is also possible in renal disease, where procainamide elimination is slowed.
Therapeutic Use
Procainamide is effective against most atrial and ventricular arrhythmias. However, many clinicians attempt to avoid long-term therapy because of the requirement for frequent dosing and the common occurrence of lupus-related effects. Procainamide is the drug of second or third choice (after lidocaine or amiodarone) in most coronary care units for the treatment of sustained ven-tricular arrhythmias associated with acute myocardial infarction.
Related Topics